Dysphagia Tips for Students &
New Speech-Language Pathologists
by Karen Sheffler, MS, CCC-SLP, BCS-S of SwallowStudy.com

As the snow melts and the first buds of spring will be coming out across the nation, graduate students who have been cramming in the data and information for years are hoping to graduate with a level of knowledge that will start them on their life-long learning quest in speech-language pathology.
They will need more than 5 dysphagia tips for students, but let’s get them started!
Read on, and if you are not a student –> ask yourselves:
- How can we support students and new clinicians, especially within this COVID-19 Pandemic and all its restrictions on education?
- How can we ensure that they build the foundation of critical thinking skills that will help them succeed?
The Students’ & Professors’ Challenges
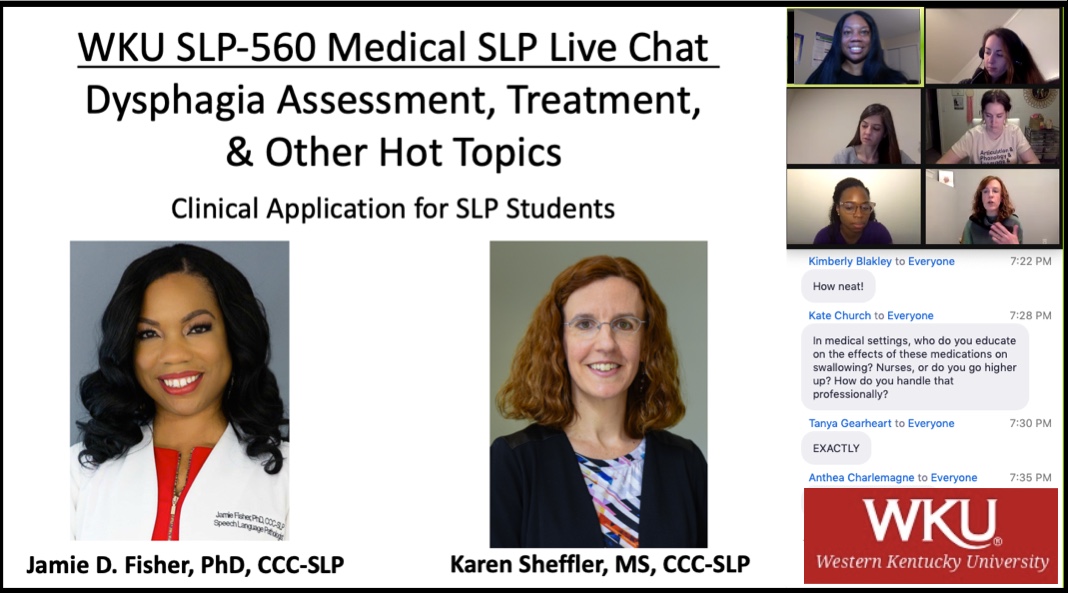
I now know there is a group of keen future speech-language pathologists at Western Kentucky University, thanks to the expert guidance of their professor and coach: Dr. Jamie Fisher, PhD, CCC-SLP.
I was honored to be invited by Dr. Jamie Fisher (see her bio at the end of this blog) to discuss hot topics, as well as to provide dysphagia tips for students in her Medical SLP Graduate level class at Western Kentucky University’s department of Communication Sciences and Disorders.
I talked with Dr. Fisher in the days after this class about how I was so impressed with how in each student shared different take-home messages that meant something to them when sending me thank-you emails. The STUDENTS were the inspiration for this blog, as many students across the world right now are struggling to complete their educations within a pandemic.
These students are resilient and are learning how to learn by any means necessary. And, it will be okay, because we need to remind our students that the goal is not to know it all upon finishing graduate school. I hope this blog, tips and resources will be helpful to guide their goal of life-long learning!
During COVID-19, we may forget the plight of these front-line graduate school professors who are trying to impart so much information and clinical experience. They want to provide the level of education that is equal to pre-COVID. Our educators must be under so much pressure. They must feel the weight of their tasks, especially since the future lives of people with dysphagia are counting on these future clinicians! Dr. Fisher reflected:
“It has been super difficult for a lot of students during the COVID-19 Pandemic with not being able to get adequate medical/clinical practicum experiences due to the COVID-19 restrictions, including students not being allowed into medical facilities. So, I’ve been trying to get as many colleagues to come in to share their experiences so students can get some real-life medical experience and learn how to make valuable connections.”
Top 5 Dysphagia Tips for Students & New Clinicians:

-
Think globally and ACT
~ Act, whether it is locally, nationally or globally ~
For examples:
-
- IDDSI.org is a great way to work locally through your facility, while connecting with other professionals nationally for resources and implementation assistance. Additionally, you will find yourself part of a global wave of standardizing dysphagia diets around the world for patient safety across all cultures, ages, and settings.
- Be involved within the field and #RaiseDysphagiaAwareness. Did you know that June is #DysphagiaAwareness month? Last year, the American Board of Swallowing and Swallowing Disorders (ABSSD) focused on raising awareness of the struggle that caregivers have when their loved one has dysphagia. Here are infographics we created.
- Use social media platforms, SIG 13 community, ASHA’s Practice Portal.
- Be involved as a volunteer in committees within ASHA, SIG 13, the Dysphagia Research Society (DRS), and through your state organizations.
- Consider working towards your board certification as a swallowing specialist (BCS-S through ABSSD – See www.swallowingdisorders.org).
NOTE: All of your extra work raises the level of your practice. Your efforts raise the collective practice standards around the nation and the world. By advocating for best practice, we can enhance how SLPs are viewed by our fellow medical professionals, while helping people who have difficulty swallowing. All of this will work to foster future research to improve how we treat swallowing disorders. We hope to find more ways in the future to rehabilitate the underlying dysphagia issues, rather than only prescribing compensatory strategies and diet modifications. We need to beef up the rehabilitative pillar of dysphagia management.
-
Always think collaboratively
Be careful! Do not trap yourself in your own dysphagia silo.
Can you imagine a supervisor urging you to do only a 10-15 minute evaluation and saying: You are the SLP here at this hospital, and you evaluate swallowing only? There are other talented professionals here for all the other aspects of the person? That would be a very narrow way of conducting yourself at work, and I would not recommend that fixed mindset.
I can name many ways where collaboration will be key throughout your workday, even though it may require a few more minutes of your time (a 15 minute dysphagia evaluation is just not realistic or safe for people with dysphagia):
-
- discussing medications with the pharmacist and geriatric specialist,
- discussing your critical findings with the team that is currently rounding on the person you just evaluated,
- seeking out the palliative care team to assist the person and family through difficult decision-making after you just educated them on the severity of the videofluoroscopic swallow study findings,
- talking with the case manager to get the person into the best-most aggressive rehabilitation center,
- educating the nurse about exactly why the swallowing strategy was effective on the study you just performed,
- collaborating with the dietitian to make sure that the meals and supplements meet with the person’s preferences and viscosity needs,
- team treating with the physical or occupational therapist to maximize positioning and head/trunk control for meals,
- working with the kitchen manager and cooks to test new recipes to increase the moisture content and cohesive nature of the Minced & Moist meals,
and many more…
This takes thinking, time, and reaching outside our SLP mindset.
Dietitians (RDN – Registered Dietitian Nutritionist) are our closest teammates in hospitals and facilities. Believe me, I never used to know what the following acronyms meant: the ANFP, the AND, or FNCE!? Do you? It helps when we know each other and speak the same language. IDDSI is helping us all speak the same language!
Think in a customer-service-oriented way. Our customers are, of course, the people with difficulty swallowing and their families/caregivers. However, our customers are also our referring doctors and other healthcare professionals. We make appropriate referrals. We reach out by phone and email to share our reports and summarize critical findings after evaluations, especially for people who are not inpatients. Ask them: who is on your team, and who coordinating your care? We are not case managers, of course, but we all need to do our part to collaborate.
-
Always question & dig deeper
Don’t be afraid to question what is written in reports in the medical records.
Review the images yourself. Open up the neck CTs, Head CTs, MRIs, and start learning how to read these.
Question yourself within your evaluations. If you find yourself only documenting residue or aspiration after your instrumental examination. Stop, and ask yourself many “why” questions to find underlying issues that made the bolus go down the wrong way or get stuck. That will help you guide your treatment recommendations so that the person can have a personalized/targeted therapy plan.
Keep in mind that the first step in treating dysphagia is making sure that all underlying medical issues are being addressed. Dysphagia is not the endpoint. It is not a disease in-and-of-itself. There is something causing the symptom of dysphagia. What is it? Ask the medical team to consider digging deeper to answer that question. We have to be okay with it being messy, as it may be multi-factorial.
Decision-making by the person, family/caregiver, and medical team has to be an informed process. Stop and ask: “Have we asked enough questions.”
Encourage your patients to ask questions. End every session with checking to see if they have any questions, making sure to ask this while you are still sitting down and not half out the door.
So, dig deep and let your documentation reflect your questioning. Ask for clarifications from the team. Ultimately, don’t be afraid to be the one who encourages slowing down a discharge by asking for further evaluations before discharge. Staying one more night is cheaper than a hospital getting a penalty for an immediate readmission when a functional nutrition/hydration plan was not adequately established before discharge.
-
Know your field’s history and research
The best thing for our relatively new field of dysphagia is when clinicians and researchers collaborate.
Therefore, know your dysphagia research from around the world (not just from the US).
Additionally, know the history within the dysphagia field, specifically those SLPs and related researchers who have passed away, such as: Drs. Logemann, Leder, Sheppard, Dodds, Donner, Sasaki…. See this blog honoring Dr. Jeri Logemann and this blog honoring Dr. Steven Leder.
Look at the names on this pdf of the Dysphagia Research Society’s (DRS) Dodds-Donner Lecture series. Start familiarizing yourself with these names, as they span the disciplines and help us SLPs get out of our own research silo. It would be really too bad if you were working for years in the field without knowing the research of: Dr. Peter Kahrilas, Dr. Reza Shaker, Dr. Peter Belafsky, Dr. Shaheen Hamdy, Dr. Bronwyn Jones, Dr. Joel Richter, Dr. Jeffery Palmer, and I could go on and on. These are just some of the major SLP allies within the fields of gastroenterology, otolaryngology, neurology, radiology, and more.
I highly recommend attending the Dysphagia Research Society meetings (now, of course virtual), as these create a multi-disciplinary meeting of the dysphagia minds. (Not to mention, we have a lot fun too).
Make sure as a new clinician, the following SLP researchers’ names start to look familiar: Drs. Arvedson (pediatric), Lefton-Greif (pediatric), Sonies (pediatric), Logeman, Rosenbek, Steele, Martino, Langmore, Robbins, Martin-Harris, Suiter, Brodsky, Humbert, Plowman, Miles, Ashford, Hegland, Troche, and so many more that I can’t possibly capture them all. Keep your eye out for newer researchers, such as: Drs. Rachel Mulheren, Sonja Molfenter, James Curtis, Ashwini Namasivayam-MacDonald, Samantha Shune, Kendra Garand, Alicia Vose, and many more.
It helps to keep active on social media to see who is sharing new research and posting new ideas/trainings. Especially follow the Dysphagia Research Society on facebook and twitter, who post every single article from the quarterly Dysphagia Journal. You can see the huge list of dysphagia researchers within this document, which shows all the Dysphagia journal’s editors: https://www.springer.com/journal/455/editors
To further familiarize yourself with new and seasoned dysphagia researchers, you can also check out the past DRS awards recepients listed here: https://www.dysphagiaresearch.org/page/past_recipients
This blog represents ways to get started as a student or new clinician, but it is very important to start reading the original research articles, not stopping at the blog or Instagram or TikTok level.
-
Reach out for help & Find mentors
Find other SLPs with whom to share ideas, ask questions, start a journal club, review cases, and develop standardized evaluations and scoring skills (e.g., MBSImP ratings).
Find mentors online and at your institutions.
Know and admit when you do not know something. That is so much better than plowing ahead, thinking you know everything. That is how even seasoned clinicians get stuck in their ways. They don’t know that they don’t know, or maybe won’t admit that they don’t know.
***
Students: Are you still hungry for more Dysphagia Tips for Students?
Then, Read On…
***
Students’ FAQ’s:
Digging even deeper into those dysphagia tips for students…
Next, I want to share the students’ emailed comments/questions (labeled STUDENT), as well as my answers and resources (labeled KAREN). I hope that this will help many graduate students and new clinicians find their way.
It is an exciting time to be entering the field of dysphagia, as new research is rapidly rolling out in this fairly new field. More research is urgently needed, especially on therapeutic methods to treat dysphagia in a targeted and person-centered way. New global standardization is underway (e.g., IDDSI.org). Finally, even with the pandemic raging for over one year, there are so many ways to obtain and digest information that do not require live-in-person meetings.
STUDENT: I really enjoyed learning about the benefits and limitations of the bedside swallow evaluation that you discussed!
STUDENT: I really liked how you pointed out the importance of knowing the history or background of dysphagia. I had not realized that in the past, SLPs relied so heavily on the bedside swallowing evaluation to determine the presence of aspiration and prescribe diets. It’s wild to me that at one-point SLPs were very focused on only diet modification (as you said: being the “diet” police), and how simply performing bedside swallowing evaluations was essentially considered the gold standard. I’m glad we are evolving and realizing that we have wonderful instrumentation such as FEES and VFSS/MBSS to help us actually see what is going on and to give us a better idea of how to treat our patients.
KAREN: It is so important to know the benefits of a bedside swallowing evaluation, as well as the limitations. Knowing your field’s history is important to not make the same mistakes or re-invent the wheel. Dr. Steven Leder, before he passed, was really trying to change the dysphagia field’s impression of the bedside. He constantly reminded us that once the mouth is closed, we cannot describe A-P propulsion or based of tongue action, we cannot “see” pharyngeal and laryngeal pathologies, we cannot know that aspiration occurred, and we cannot confidently comment on what is happening once that bolus is out of sight. We cannot confidently document about the efficiency of the swallow (residue) and the safety of the swallow (airway compromise – penetration/aspiration). We cannot be sure about our diet recommendations based solely on the bedside swallowing evaluation. We have to say what we “suspect” to be a risk or problem. We do often have to make urgent-temporary modifications based on our best clinical judgement, especially for those who are hospitalized and critically ill. We may recommend a potentially “safer” diet for those who will receive an instrumental evaluation the next day or later in the week. Again, these diet changes are recommended based on our best judgement for the person’s immediate safety concerns.
However, we have to document the exam’s limitations too. We have to document our rationales for whether further assessment is necessary or not. We have to ensure that the other medical team members understand that the bedside swallowing evaluation has limitations. Too many other professionals, and even lawyers, think what we say is The Word! They think we have x-ray goggles! That has led to many healthcare providers and administrators thinking that they don’t have to send patients for instrumental evaluations. Facilities don’t want to pay for the studies’ added costs if they think we have bedside x-ray goggles and can know-it-all. We must advocate for our instrumental evaluations to guide our treatments. Otherwise, it would be like treating all respiratory distress, cognitive-communication changes, and falls without chest x-rays and chest CTs to rule out pneumonia or lesions, without MRIs to rule out strokes, and without hip imaging to rule out fractures.
All that said, though, I still never call our clinical bedside swallowing evaluation a “screen,” or even a “bunch of screens,” as some SLPs have described it in the past. See my “Dishing on Dysphagia” ASHAsphere article – section 2 talks about what a clinical bedside swallowing evaluation (CSE) can and cannot do.
Think about all we do with our critical thinking caps on: thorough chart review, interviews of the person with difficulty swallowing and all family/staff involved, cranial nerve exam, oral and dental inspection, cognitive-communicative eval, speech-voice assessment, and finally the oral intake trials or meal evaluations. All of these pieces are so crucial parts of the puzzle. They create our hypotheses about the person’s case. They give us direction to help focus the dysphagia evaluation’s next steps. We are the deglutologists, as I stated in class, that can help save healthcare dollars by targeting the evaluation. We can help guides the appropriate referrals. Otherwise, I have seen many primary care physicians take shots in the dark, sending a person to many people and many different examinations without a clear focus.
Our bedside swallow evaluation also gives us the rationale behind whether the person needs an instrumental or not. Not everyone you evaluate will need further testing. Additionally, that initial rapport building with the person and their family/caregivers is also very important. We don’t want to dictate to them our recommendations, we want to build a relationship so that we and the medical team can have conversations about options.
All that is way more than a screen.
Even the definition of a screen is a tool that can be done by anyone on the normal population to find those who may have a problem. Whereas, the person you are performing a bedside swallowing evaluation on was referred to you by the medical team with an order. That order should elude to the question the medical team has about that person’s oral intake. Answering the medical team’s questions in a report is certainly not a screen! Would we call a doctor’s initial H&P (history and physical examination done without fancy instrumentation) a screen? No. Finally, we can’t call it a screen when it is what we do every day at hospitals through home healthcare, as we are putting so much into these bedside swallowing evaluations. We do deserve to charge insurances and make a good salary. Would we be calling what we do a “bunch of screens” if our profession was majority male versus majority female? (Had to ask that too!)
On your other point, it is so great that students are learning now from the start that therapy has to be targeted to the individual, and the only way to do that is to use our instrumental evaluations (FEES and VFSS/MBSS) to determine the underlying pathophysiology and structural issues causing the dysphagia and aspiration. We have to ask, “why?” many times to figure out what caused the bolus to do what it did. We do not document about the bolus, we document about the person and what we can do about the dysphagia issues we find. I mentioned Dr. Ianessa Humbert, whose course years ago called “Critical Thinking in Dysphagia Management” really got us asking Why – at least 5 times for each issue in an exam – to dig deep into the underlying problems. I also mentioned how she now has her Masterclass in learning about normal swallowing (see link in the resources list below). We have to understand all the variances in normal swallowing to really analyze the disordered swallow well.
***
STUDENT: The information you provided was truly impactful in how we as novice clinicians can begin to interact with the literature that is currently out about dysphagia. You also highlighted some ways to better understand medication and its effect on patient and potential reason why they have dysphagia, while simultaneously getting in the good graces of physicians.
KAREN: You made several great points there. Regarding literature, please see my 10 articles and resources at the end of this blog, but don’t stop there. Read primary source articles.
I am going to go more into your point regarding our collaboration with the medical team (i.e., physicians, nurse practitioners, physician’s assistants). Dr. James Coyle, PhD, CCC-SLP, BCS-S (a prominent SLP clinician and professor from University of Pittsburgh) has been saying that SLPs need to be trained more like medical doctors. How else will we know this completely different medical lingo? (It is like a new language.) We need to know the ins and outs of many different diseases and disorders, as well as the big picture ramifications of all of our decisions and recommendations? Many discussions we have with people and their doctors are regarding the risks and benefits of every decision they are making. People (patients) are drivers of their own healthcare teams, but they need us to be knowledgeable enough to contribute intellectually and sensitively to the discussions. It takes a lot of critical thinking skills. It also takes enough knowledge and training to know what you don’t know, and when you need to seek help. The most dangerous situation is not knowing that you don’t know something. Then you may continue to do things the “old way” or the way you have always done it, because you have not kept up with the latest evidence.
Another point to make in our interaction with the whole medical team, is that we cannot dictate our one “perfect” recommendation. As we joked in class, we are not the “diet police,” mandating the one diet change that we think is best. Your recommendations can have a big impact. For example, if you say “NPO” (recommending nothing by mouth), this may corner the doctor into just trying to convince the person and family/caregiver into one decision of placing a feeding tube, rather than prompting a conversation. Whereas, if we provide options and suggest that the team has goals-of-care discussions, then we leave the doors open for an open-ended conversation! We provide options to consider within a range of:
- super cautious and more aggressive approaches (e.g., attempting to mitigate aspiration and choking risks to the greatest extent possible)
—> through —>
- less cautious and more palliative or quality of life focus (e.g., continuing oral intake per the person’s preferences and comfort, with attempts to mitigate infection with mobility and good oral infection control).
It is a spectrum that we can help the whole medical team understand, including the person with dysphagia and their family/caregiver/healthcare proxy.
Ultimately, for our work, we have to code switch a lot. We need to talk the same language as the doctors, NPs, PAs, and other healthcare professionals, while speaking clearly to the people we serve. We need to let the doctors know that we are thinking of details as well as the big picture. When we ask good questions and offer valuable insight, we are included in the whole medical team. To keep conversations open about further testing, we need to let the doctors and the people with dysphagia know about the limitations of our bedside examinations. Consider checking out this blog about the necessary collaborations between SLPs and palliative care: https://swallowstudy.com/conversation-slp-role-palliative-care/
IDDSI is only one example of being able to finally speak the same language with its standardized framework of diet labels and descriptors.
***
STUDENT: Thank you for taking the time to speak with our class last night! I learned so much, and I especially loved the CYA acronym.
KAREN: Ah, yes, the “CYA” acronym or covering your backside. We have all used that in medicine. However, when we say CYA, what we are really ensuring is that we are providing the best, evidence-based, and most thorough care for that person that we can. Ultimately, what covers you in your practice is what is best for the person with dysphagia. So, again, by providing good patient care, we are automatically protecting ourselves. However, our documentation has to reflect all of our good work. In litigation, we are held to a benchmark of a “reasonable or prudent standard of care,” but why not go beyond that? We can strive to excel and move the field forward in the level of care that SLPs provide.
Providing excellent and exceptional care requires:
- critical thinking,
- good documentation that provides the rationale of why you chose to do what you did,
- collaboration,
- good communication,
- training others,
- teaching/counseling our patients/caregivers/family, and
- ensuring a continuity of care from hospital to nursing facility or from facility to home.
If you do those things, you are working at the top of your license (as Theresa Richard, MS, CCC-SLP, BCS-S from the MedSLP Collective and “Swallow Your Pride” podcast describes. See “Swallow Your Pride” podcast links in resources below).
Once you really dive into the field of dysphagia for a few years, you can become certified as a swallowing specialist by the American Board of Swallowing and Swallowing Disorders (ABSSD). The ABSSD certifies speech-language pathologists with the BCS-S, or Board-Certified Specialist in Swallowing and Swallowing Disorders. This shows that you have specialized and advanced skills within the field of swallowing and swallowing disorders. Check out at www.swallowingdisorders.org, get on a roughly 3 to 5-year track as a newer clinician, obtain a mentor, and make a plan for your achievement of excellence as a dysphagia clinician.
***
STUDENT: I was hoping you could tell me about the High-Flow Oxygen Nasal Canula and how it affects swallowing and may increase a risk for dysphagia. Today, at my externship placement, we completed a bedside swallowing assessment for a patient using a HFNC. The person had COVID-19 who was discharged from the hospital less than 2 weeks ago and was readmitted due to breathing difficulties. His respiratory rate (RR) seemed to stay between 25-30. Is there research out there that gives us definitive answers stating that the HFNC causes dysphagia?
KAREN: Unfortunately, there is no good-quick answer yet about HFNC. This is a good example of how dysphagia research is in its infancy, and it is such a good time to be in the field and continue to question everything! We can support organizations that advance the science of dysphagia, such as the Dysphagia Research Society (DRS) – www.dysphagiaresearch.org.
And here is my monster blog on High Flow Nasal Cannula (HFNC), for which you will need either a cup of coffee or a big glass of wine while you process it!! I write very lengthy blogs!
https://swallowstudy.com/high-flow-nasal-cannula-hfnc-does-it-increase-dysphagia-aspiration-risk/
In an attempt at a brief summary to your questions, when a person’s RR is over 25, the person may have difficulty coordinating breathing and swallowing. (See this blog also on critical values.) The act of swallowing requires a “swallow apnea” period, or better described as a cessation of breathing while swallowing. Dr. James Coyle* advises that when a RR is above 25, we should pay close attention for breathing-swallowing coordination concerns. People who have a rapid breathing rate will tend to have irregular breathing patterns while eating/drinking. They may breathe in after the swallow, rather than the safer pattern of exhale – swallow- exhale. (See research by Drs. Bonnie Martin-Harris and Roxann Diez Gross – I will link to Gross’s, 2009 article, as her name is not as common out there as Dr. Martin-Harris). Of course, breathing in after the swallow could suck in any material sitting in the top of the laryngeal vestibule or any residue leftover after the swallow that is near the airway. Regarding the decision-making that we do when evaluating a person on HFNC, please check out the issues posed in my HFNC blog above, as well as the chart of suggested guidelines at the end. Your question is a tough one that cannot be answered simply. (You will hear this again and again in your career, as there are no clear black-and-white answers). The bottom line is that every person on HFNC has to be considered individually. Please share with others your findings. Research can even be single-subject design.
(*You may see from my blogs, I talk about Dr. James Coyle a lot. He really is one of the great SLPs to listen to in webinars/seminars. And, I’d like to think my dysphagia humor started with him as my university teacher. Here is one of my early blogs inspired by a talk of his: https://swallowstudy.com/aging-and-swallowing-we-all-have-to-do-it/)
***
STUDENT: I really enjoyed listening to your perspective and experience with dysphagia. I was interested in your information you presented on medications and the influence on dysphagia with patients. I did not have much knowledge of this prior to hearing you speak and will make it a priority to do more research on this to become more well informed.
STUDENT: I appreciate you coming to our class last night and enjoyed hearing your passion for your job. I also want to thank you for all the good resources you provided us. Those will come in handy as I start my career. When you spoke about cheat sheets of charts on your clipboard, that is definitely something I am going to do, especially with the medications that could impact swallowing.
KAREN: As I said in class, even seasoned clinicians may carry charts around with them (in paper or electronically) to double check facts, data, research, and those crazy cranial nerves. You may frequently second guess yourself on details, and that is okay. When you know where to access information, you are really ahead of the game. When we are putting information into a medical record, we want to make sure we are being as accurate as we can be.
Additionally, we can cite research in the medical record to support our documentation. For examples, when your facility specifically uses the Yale Swallow Protocol for a stroke swallow screen, you would cite: Leder, S.B & Suiter, D.M. (2014). The Yale Swallow Protocol: An Evidenced-Based Approach to Decision Making. Springer, NY. If you are performing a 3-ounce water challenge and want to make the point that people do not often silently aspirate when consuming large volumes of water rapidly without stopping, you could directly cite in the medical record: Leder, et al., 2011. (Leder, S.B., Suiter, D.M. & Green, B.G. (2011). Silent aspiration risk is volume dependent. Dysphagia, 26, 304-309.)
Here are some of those chart links we talked about:
- There is a cranial nerve chart in pdf form on my website within this link:
https://swallowstudy.com/crazy-cranial-nerves-swallowing/
- The medication chart is in this link to my blog on drug-induced dysphagia:
https://swallowstudy.com/abas-drug-induced-dysphagia/
***
STUDENT: I am currently placed at a SNF for my clinical rotations. I have noticed that our patients on modified diets often have snacks that lack variety and enjoyability compared to the snacks residents on a regular diet receive. That being said, your blog post titled “Snacks for People with Dysphagia (IDDSI Style)” was so helpful to me and I will definitely be taking these suggestions back to my supervising SLP at my placement!
KAREN: Thank you for reading my blogs! The one you mentioned – https://swallowstudy.com/snacks-for-people-with-dysphagia-iddsi-style/ – can be helpful for clinicians to meet the person’s food preferences and quality of life needs. I wanted to extra point out, though, what Dr. Catriona Steele highlighted at the end of that blog. IDDSI uses a framework to provide clear descriptions and testing methods to make sure a given food item is appropriate for a given diet level. In the past, the National Dysphagia Diet (NDD) provided an American-focused list of foods “allowed” on a given diet level. However, IDDSI is not so prescriptive and narrowly focused. It is descriptive with testing methods that can be easily done, even within the home kitchen of the person with dysphagia (e.g., Spoon Tilt Test & Fork Pressure Test). IDDSI provides an internationally applicable and descriptive framework to help standardize dysphagia diets for safety across all regions, all care settings, all ages, and all cultures. Therefore, you could work with your supervisor, the facilities dietitian and the kitchen staff to individually test the recipes and snack products to make sure they are appropriate for your modified diets.
Note: it was a student SLP in 2016 at the large hospital where I work who initially kicked off our IDDSI Awareness and Implementation phases. See Laina Piera’s article here: https://doi.org/10.1044/leader.OTP.24042019.38
Students can make a difference!
***
STUDENT: Thank you so much for taking time to speak to our class on Monday evening. You had so much good insight and advice I had not heard yet! I was so intrigued; I didn’t even realize class was running over! I appreciate all the resources you provided to us, but my biggest take away from your presentation was that we should not limit ourselves to just SLP knowledge.
KAREN: Yes, it is so important to get out of ourselves (out of our dysphagia silo or SLP silo) and collaborate with other disciplines. I am working with dietitians and food service professionals on a weekly basis, especially within my work with IDDSI’s USTIRG (United States & Territories IDDSI Reference Groups), which are supporting the implementation of the International Dysphagia Diet Standardization Initiative (www.IDDSI.org). IDDSI is a great example of the need to work globally and across disciplines (which is also the focus of the Dysphagia Research Society). IDDSI is made up of volunteer researchers, clinicians, scientists, and other healthcare professionals from around the world. The collaboration even reaches into material science and mechanical engineering, regarding the study of the flow of materials (rheology) and fluid dynamics in our working with liquids of different viscosities. Our field is so broadly reaching and very exciting!
Another great example of stepping out of our SLP field, as well as out of our country for enrichment is: in mechanical engineering with Dr. Ben Hanson’s work. Dr. Hanson is from from the University College of London (UCL) in London, England. Per the UCL’s website:
“He specialises in biomedical engineering and researches how the body’s mechanical control systems work. His two main themes are cardiovascular arrhythmias and the biomechanics of eating & drinking.”
Check out his video on viscosity here: https://mecheng.ucl.ac.uk/benhanson/homepage/publications-articles-videos/. On that website page, you can see a picture of his tongue model across the top banner. He is studying how the tongue’s motions and pressures interact with different fluid bolus viscosities. He also invented the IDDSI Flow Test, which is helping us standardize and test the levels of liquid, such as: thin liquid, slightly thick liquid, mildly thick liquid (old term: nectar thick), moderately thick liquid (old term: honey thick), and extremely thick liquid (old term: pudding thick or spoon thick).
An additional point I must make regarding regarding collaboration and medications and dysphagia is how pharmacists are quite underutilized in hospitals and ICUs everywhere. We as SLPs can contribute so much by suggesting other team members to bring to the table for the good of the individual. Pharmacists, the palliative care team, and geriatric specialists, to name a few, are certainly frequent referrals we may suggest.
***
STUDENT: I learned so much from the wonderful resources you provided and the class discussion. There were many historical names on the list I had never heard before, and I look forward to learning more about these leaders in our field. One thing I particularly found interesting from our discussion was how patients are not good at localizing where their problem lies and how this fact also places importance on doing an instrumental.
KAREN: Thank you for your interest in our field’s history. You can see some of the names I mentioned in the 5-Tips section above.
Regarding people’s ability to localize where foods, liquids and pills get stuck: Here is that Stevie Marvin article I mentioned in class. (Marvin & Thibeault, 2019: https://pubs.asha.org/doi/pdf/10.1044/2019_AJSLP-19-00161)
People have difficulty localizing where a bolus is stuck (i.e., where within the esophagus or even whether the food or pill is stuck in the esophagus versus the throat/pharyngeal regions). People will generally point to neck area when they feel food or a pill stuck. Many people can become really fearful and think they will choke. Many people come to us after a long time of restricting their intake. We can reduce fear, potentially liberalize intake, provide effective strategies/counseling, and improve their quality of life. We can do all this by performing the videofluoroscopic swallow study with food, liquid and pills, while scanning down the esophagus on each type of bolus. (See this blog on multi-phase dysphagia evaluations). Then, sometimes, just by showing them the video image during and after the study, we can alleviate their fears of choking. We can show them where the problem actually is. If the food is stuck at the bottom of the esophagus, they should not be so fearful of actual airway blockage or choking. The SLP can lead the person with esophageal dysphagia in the direction of GI to further perform differential diagnosis and treatment (with esophageal scoping/EGD, barium swallow studies, and manometry). I should emphasize, we don’t diagnose problems in the esophagus, but we can see how esophageal dysphagia impacts on the bolus flow and level of risks. We then provide interim strategies and counseling while the individual is waiting for further testing with GI and/or radiology.
At the bedside, pay attention to when people vaguely point to neck. Make them choose one spot, if they can. If that spot is really in that lower neck notch area, then it is more likely a food stasis (food sticking) in the esophagus. Ask, does it work to wash food down with liquid? Does it happen more so on bread and meat? When you try to wash it down and/or drink quickly, does liquid shoot back up into your throat? All these answers will help you focus your evaluation. You will need a videofluoroscopic swallow study to scan down and differentiate between oropharyngeal, pharyngoesophageal, or esophageal. We have to dive into esophagus as it directly affects the whole swallow. We can see supraesophageal reflux or esophageal backflow on FEES also, but you cannot see below to determine potential underlying causes. Remember when Dr. Fisher showed that FEES examination video and the green pudding came back up into the bottom of the throat/hypopharynx after the swallow? That esophageal backflow can be primary cause for aspiration after the swallow, and it can lead to complications like choking and aspiration pneumonia.
Note: The risk for aspiration pneumonia would be higher in a person who also had other issues, such as: bedridden status, poor host immune response, and pathogenic bacteria buildup in oropharyngeal cavities. I am sure Dr. Fisher has or will go over Dr. Susan Langmore’s work on the predictors of aspiration pneumonia and Dr. John Ashford’s pillars of aspiration pneumonia (See resources below).
Too many SLPs will tell you the esophagus is not our scope of practice, but it really is. See this Scope of Practice document from ASHA in the “Domains” category: https://www.asha.org/policy/sp2016-00343/.
I hope my brief introduction to esophageal dysphagia was helpful and starts you on your journey. Please also see these blogs on the esophagus: How Low Do You Go? Esophageal Dysphagia and Dysphagia Digest: Multiphase Dysphagia Evaluations.
***
STUDENT: A wealth of knowledge with a fun approach, I could have listened all night!
I was taking notes like crazy and can’t wait to dive into the resources you provided to us.
STUDENT: I also really appreciate you sharing your favorite articles, podcasts, STEP program information, oral infection control, and your 5 valuable tips. I have spent lots of time this week eagerly going over the resources you provided, thanks!
KAREN: These students are learning that graduate school is just the beginning of our life-long learning, as noted by Ainsley Martin, MS, CCC-SLP in this blog, written when she was a fairly new clinician.
Dr. Fisher asked me to share just a few of my favorite research articles and resources. I cannot say these are my “top-10,” because how would I ever stop at just 10!
I hope other clinicians can share resources at the end of this blog, so that future students can benefit.
Dysphagia Resources for the Student & New SLP
1. Predictors of aspiration pneumonia: I must recommend the dysphagia field altering research by Dr. Susan Langmore and her team in 1998 and 2002. Dr. Langmore and colleagues created lists of the predictors of aspiration pneumonia. While these factors do not show causation, there were crucial predictors that correlate strongly with aspiration pneumonia, such as dependency for eating and oral infection control (oral hygiene), having multiple medical diagnoses, and a bedridden status.
-
- Langmore, S.E, et al. (1998). Predictors of aspiration pneumonia: How important is dysphagia? Dysphagia, 13, 69-81.
- Langmore, S.E, et al. (2002). Predictors of aspiration pneumonia in nursing home residents. Dysphagia, 17 (4), 298-307.
2. International Dysphagia Diet Standardisation Initiative (IDDSI): Please see all the publications & resources on the need for dysphagia diet standardization by IDDSI.org: https://iddsi.org/Resources/Publications
-
- I also have many blogs on the topic: See IDDSI Resources,
- My first IDDSI blog: Diet Safety: Terminology & Definitions Matter, and
- The topic of mastication evaluation that often goes under-evaluated: Diet Modification Without Mastication Evaluation?
3. The High Cost of Dysphagia – which often goes under-identified, under-referred, under-evaluated, and under-treated. D.A. Patel,S. Krishnaswami,E. Steger, E. Conover, M. F. Vaezi, M. R. Ciucci, D. O. Francis (2018). Economic and survival burden of dysphagia among inpatients in the United States. Diseases of the Esophagus, 31, 1-7. DOI: 10.1093/dote/dox131
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6454833/pdf/dox131.pdf
4. The need for instrumental evaluations: Miles, A., McFarlane, M., Scott, S. & Hunting, A. (2018). Cough response to aspiration in thin and thick fluids during FEES in hospitalized inpatients. Int J Lang Commun Disord., 53(5), 909-918. doi: 10.1111/1460-6984.12401. Epub 2018 May 30. PMID: 29845700. https://pubmed.ncbi.nlm.nih.gov/29845700/
-
- Miles & colleagues showed how a person may “overtly aspirate” thin liquid (showing a cough), while sometimes going on to silently aspirate the subsequent trials of nectar thick/mildly thick liquid. The person’s response is not always viscosity dependent!
- Oliva Both, from this WKU class shared her thoughts and fears about how patients can
“show overt signs of aspiration, such as a cough, during the thin liquid trial, and then have silent aspiration during the nectar thick (mildly thick) trial. This was pretty surprising to me and honestly pretty scary, because I see a lot of patients in acute care who we have been put on nectar thick because they clearly showed overt signs/symptoms of aspiration on thin liquids. It seems that it is a lot harder to schedule FEES or VFSS/MBSS for patients in acute care than patients in outpatient care because of how quickly they come and go. It definitely gave me something to think about.”
-
- Therefore, if you suspect dysphagia and aspiration risk, it is wise to proceed with and advocate for an instrumental evaluation, as your bedside judgement entails a bit of guesswork. The instrumental evaluation:
- guides your dysphagia diagnosis & severity,
- identifies safety (airway invasion) and efficiency (details) details,
- identifies why the bolus did what it did (because we don’t treat a bolus!), and
- targets your treatment plan, which includes diet modification but also targeted therapeutic exercises to allow for recovery.
- Therefore, if you suspect dysphagia and aspiration risk, it is wise to proceed with and advocate for an instrumental evaluation, as your bedside judgement entails a bit of guesswork. The instrumental evaluation:
5. Regarding medications and drug-induced dysphagia:
-
- See my drugs and dysphagia article/resources (https://swallowstudy.com/drug-induced-dysphagia-resources-safe-practices/), as well as my
- Webinar on Summit Education (https://summit-education.com/course/GPHAKS.1/medications-drug-induced-dysphagia-complications-and-potential-treatments#/onlinevideo/2-ceus (Financial Disclosure: I receive commission on sales of webinar).
To dive into this topic a bit more, I shared the following information with students about how SLPs can start thinking about pharmacological interventions, as well as the overuse of antipsychotics for people with delirium.
- Per the American Geriatric Society’s 2015 guidelines, pharmacological interventions should only be considered in cases of severe agitation and need to prevent harm to oneself or others, starting with lowest possible dose, after all other strategies have failed. The SLP, OT, and PT can help with these non-pharmacological methods to reduce agitation and delirium.
- Delirium: John’s Hopkins, Baltimore has done a lot of recent research on the inappropriate use of antipsychotics for people with delirium. Hopefully, the tide will start turning away from the use of Haldol for prevention and treatment of delirium, as it can cause dysarthria, drooling, dysphagia and other extrapyramidal side effects (EPS).
- Neufeld, et al. (2016). Antipsychotic medication for prevention and treatment of delirium in hospitalized adults: A systematic review and meta-analysis. JAGS.
- Per Johns Hopkins (Follow @ICUrehab on Twitter): Current evidence does not support routine use of haloperidol or second-generation/atypical antipsychotics to prevent or treat delirium in adult inpatients, per systematic reviews comparing the two classes of antipsychotics versus placebo.
- Prevention article: Oh, et al., 2019, Sept: https://annals.org/aim/fullarticle/2749494/antipsychotics-preventing-delirium-hospitalized-adults-systematic-review;
- Treatment: Nikooie, et al., 2019 https://annals.org/aim/fullarticle/2749495/antipsychotics-treating-delirium-hospitalized-adults-systematic-review
- 400+ page pdf of full project: https://effectivehealthcare.ahrq.gov/sites/default/files/pdf/delirium-finalreport.pdf
6. The cautions of prolonged NPO: Here is a good article on the need to keep people who are undergoing chemoradiation eating by mouth. People with head/neck cancer who are able to maintain at least a little bit of oral intake through their treatment are keeping their muscles active. They do better than those who are kept NPO through chemoradiation. Keep them moving! SLPs need to collaborate with the team to reduce pain and keep the oral condition top notch, as if people are suffering from severe oral pain and mucositis, they won’t eat and exercise the muscles.
-
- Langmore, S., Krisciunas, G.P., Miloro, K.V., Evans, S.R, Cheng, D.M. (2012). Does PEG use cause dysphagia in head and neck cancer patients? Dysphagia, 27(2), 251–9.
7. Don’t forget to collaborate with other disciplines and look at research from other fields and other countries. Here are two examples:
- Dr. Madison Macht (pulmologist/critical care specialist) has great work regarding swallowing from the ICU/critical care perspective. As stated below in his “Swallow Your Pride Podcast,” SLPs and Pulmonologists should be like peanut butter and jelly. We go together.
- Macht, 2014, swallowing dysfunction after critical illness: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4251623/
- List of Macht’s research on pubmed: https://pubmed.ncbi.nlm.nih.gov/?term=Macht%20M%5BAuthor%5D&cauthor=true&cauthor_uid=25451355
- Macht on Swallow Your Pride Podcast: https://www.mobiledysphagiadiagnostics.com/040-madison-macht-m-d-why-slps-and-mds-should-be-like-peanut-butter-and-jelly-and-the-fallacy-that-feeding-tubes-prevent-aspiration/
- Swallow Your Pride Podcast show notes: https://www.mobiledysphagiadiagnostics.com/wp-content/uploads/SYP-Episode-40.pdf
- See also my blog on Dr. Joel Ritcher, MD, FACP, MACG, who feels that SLPs are the perfect discipline to lead swallowing evaluations, as we can come from all angles to direct the essential evaluations and treatment.
8. PODCASTS are a great way to multi-task your dysphagia learning:
- Theresa Richard’s “Swallow Your Pride” Podcast. Here is one link to listen to Dr. James Curtis, a newer researcher you can follow on the social media platforms too! https://podcast.theresarichard.com/tag/james-curtis/
- Dr. Ianessa Humbert & Alicia Vose’s “Down The Hatch” Podcast, which has since ended. Check out this favorite on documentation:
9. STEP (Swallowing Training and Education Portal): Dr. Ianessa Humbert has always stressed the importance of understanding the normal swallow in addition to lots of critical thinking. Consider checking out this Swallow Physiology Masterclass: https://www.stepcommunity.com/pages/masterclass. I have nothing to financially disclose here, but I did do peer review for this program (volunteer).
10. All things Oral Infection Control:
- See Dr. John Ashford’s work and a nice podcast to review it:
- See many oral infection control blogs on this website. Links within this blog.
- I will have a free webinar on NFOSD March 25th, 2021: https://swallowingdisorderfoundation.com/webinar-oral-care/
Summary of Dysphagia Tips for Students & New Clinicians
I will close this blog with words from a student, Jennipher Burnett:
“The field of speech-language pathology is so vast. I appreciate the information you shared and the perspective you provided.
I love that you started your talk with the importance of “person-first” treatment. Our patients are people first with families, jobs, hobbies, dreams, and more. The best possible care we can provide takes all of that into account. I am completing my medical externship with a home health SLP, and I have seen firsthand how treatment really centers on who the person is and what is important to them. I also was so interested in your experience as an expert witness in litigation. You provided us with an understanding that if something isn’t written in your documentation, then that thing did not happen. That is critical in protecting those we evaluate/treat and ourselves in our future careers.
Thank you again for taking the time to speak to us. As I look back on my education, I have so many wonderful educators and SLPs that have invested in me through education, supervision, and/or mentoring. Your passion for your job was contagious, and I am fortunate to have your name on that list.”
Please add your seasoned advice and resources to this blog. Provide your own dysphagia tips for students and new speech-language pathologists. Be that mentor for new clinicians now, especially in these challenging times…
*******
Thank you to Dr. Fisher and her medical SLP class at Western Kentucky University for this blog’s inspiration!
 Jamie D. Fisher, PhD, CCC-SLP is owner, speech-language pathologist (SLP), endoscopist, and CE-training course director at Nashville Speech & Swallowing Specialists, PLLC. Dr. Fisher has served as adjunct professor at Western Kentucky University, Jackson State University and the University of Maryland – College Park. She received her PhD in Speech-Language Pathology from Vanderbilt University. She has SLP licensure in multiple states and has experience working in acute care hospitals, sub-acute care facilities, rehabilitation facilities, school districts and private practice with adults and children across America. Dr. Fisher holds American Speech-Language-Hearing Association Certificate of Clinical Competence, endorsement for endoscopy practice, and is a certified endoscopy trainer of Fiberoptic Endoscopic Evaluation of Swallowing (FEES). She has over fourteen years of experience as a SLP and her clinical interests include speech, language, literacy, dysphagia, FEES/Modified Barium SwallowStudy.com, and working with patients requiring tracheostomy/mechanical ventilation. Dr. Fisher is the creator and director of Preparing SLPs for Tracheostomy and Ventilator Patient Care Training Course in Nashville, Tennessee. She is also the co-creator and co-director of The Medical SLP Clinical Symposium at Johns Hopkins Hospital in Baltimore, Maryland.
Jamie D. Fisher, PhD, CCC-SLP is owner, speech-language pathologist (SLP), endoscopist, and CE-training course director at Nashville Speech & Swallowing Specialists, PLLC. Dr. Fisher has served as adjunct professor at Western Kentucky University, Jackson State University and the University of Maryland – College Park. She received her PhD in Speech-Language Pathology from Vanderbilt University. She has SLP licensure in multiple states and has experience working in acute care hospitals, sub-acute care facilities, rehabilitation facilities, school districts and private practice with adults and children across America. Dr. Fisher holds American Speech-Language-Hearing Association Certificate of Clinical Competence, endorsement for endoscopy practice, and is a certified endoscopy trainer of Fiberoptic Endoscopic Evaluation of Swallowing (FEES). She has over fourteen years of experience as a SLP and her clinical interests include speech, language, literacy, dysphagia, FEES/Modified Barium SwallowStudy.com, and working with patients requiring tracheostomy/mechanical ventilation. Dr. Fisher is the creator and director of Preparing SLPs for Tracheostomy and Ventilator Patient Care Training Course in Nashville, Tennessee. She is also the co-creator and co-director of The Medical SLP Clinical Symposium at Johns Hopkins Hospital in Baltimore, Maryland.


Thank you so much for all the information again. This blog highlights what you provided in the our class, including all the research articles which I love!! Research articles allow for efficacy in practice/treatment, buy in with patients and family, and buy in/referrals from the physicians which will consistently keep our profession afloat. Read the research articles (I’m still trekking my way through all the glorious information)!! 🙂
I am bookmarking this post for future reference. Once again, you came through with some great advice and I look forward to implementing your tips as I head toward graduation and beyond. Great post and advice Ms. Sheffler!
This advice was extremely useful. First and foremost being told it’s ok not to know everything when we leave graduate school is relieving; there is so much I have been taught but still so much more to learn. IDDSI.org was a great resource on standardizing dysphagia diets and one I will use in my career. I think it is easy to focus on the patient and forget about the burden the family and caregivers are shouldering. I have seen this personally watching my mom try to care for my dad. Thank you for addressing it and giving us resources to focus on caregiver burden and possibly reduce it, I have bookmarked them for future reference!
Raising the level of practice through advocating best practice can enhance the way SLPs are viewed by fellow medical professionals, while helping people who have difficulty swallowing. There are some places (SNF’s I’ve heard of most often) that rely solely on bedside evaluations instead of instrumentals. It has made me hesitant to work in an SNF, but I want to advocate for those patients who are often on long term modified diets, often for the comfort of the SLP or family with no real evidence of a need. To do this I would try to impress upon the facility that we do not have x-ray glasses and cannot definitively say that a person has dysphagia without an instrumental, and give them a list of the research (which I found on swallow your pride) but what if they still don’t see a need for instrumental evaluation? What is your suggestion in that situation? Is it ethical to treat someone long term for dysphagia without an instrumental or pathophysiological finding?
Excellent question to bring in ethics! Keep advocating – you are on the right track with your good critical thinking.
Ask the team, would you treat hip pain after a fall without imaging? That is unethical, right?
We need to raise our standards and professionally raise our voices to advocate for best practice – whether that is IDDSI or getting good imaging to guide our targeted person-centered treatment. Additionally, we at IDDSI are working on handouts for all stakeholders (like administrators) to help them see the risks and costs of pneumonia, choking, and other negative sequelae. Those risks/costs are far greater than costs of a VFSS, FEES, or even an adequate oral hygiene/oral infection control program. It is unfortunate to focus on money rather than our patients, but sometimes it is showing the monetary costs that may help you advocate within administration.
This advice was extremely useful. First and foremost being told it’s ok not to know everything when we leave graduate school is relieving; there is so much I have been taught but still so much more to learn. IDDSI.org was a great resource on standardizing dysphagia diets and one I will use in my career. I think it is easy to focus on the patient and forget about the burden the family and caregivers are shouldering. I have seen this personally watching my mom try to care for my dad. Thank you for addressing it and giving us resources to focus on caregiver burden and possibly reduce it, I have bookmarked them for future reference!
Raising the level of practice through advocating best practice can enhance the way SLPs are viewed by fellow medical professionals, while helping people who have difficulty swallowing. There are some places (SNF’s I’ve heard of most often) that rely solely on bedside evaluations instead of instrumentals. It has made me hesitant to work in an SNF, but I want to advocate for those patients who are often on long term modified diets, often for the comfort of the SLP or family with no real evidence of a need. To do this I would try to impress upon the facility that we do not have x-ray glasses and cannot definitively say that a person has dysphagia without an instrumental, and give them a list of the research (which I found on swallow your pride) but what if they still don’t see a need for instrumental evaluation? What is your suggestion in that situation? Is it ethical to treat someone long term for dysphagia without an instrumental or pathophysiological finding?
This is a duplicate question – Thanks Victoria – and please see my answers below.