Jelly & Jell-O Surprise: Jell-O, Jelly Cups, Dysphagia Training Jelly
(Transitional Foods Blog Part 3 of 3) By Karen Sheffler, MS, CCC-SLP, BCS-S of SwallowStudy.com with special contributions by Mari Kato-Nakao, MD, MA, (PhD candidate) on Japanese Dysphagia Training Jelly
Introduction
Maybe you were just saying: “You had me at the Jell-O,” but I am not talking about Jell-O shots!
You are tuning in for Part 3 of my three-part series on how Transitional Foods affect someone who has difficulty swallowing (dysphagia).
“Transitional Food” is a special category in the globally standardized dysphagia diet framework called IDDSI or International Dysphagia Diet Standardisation Initiative (www.IDDSI.org).
Part 1 provided plenty of information about transitional foods and testing methods.
Part 2 discussed patient safety and public safety around swallowing and choking risks. For example, I exposed the potential choking risks with foods that may have been marketed as transitional foods or first finger foods for infants.
In Part 3, we will explore:
- Transitional foods that are extra challenging for people with dysphagia (e.g., gelatin and Jell-O) and some potential product solutions.
- Discuss Japanese Konjac Jelly (aka, Conjac, Congac, Konjac Candy, Konnyaku, Mini-cup Jelly cups, glucomannan), which has been taken off the market in the United States by the Food & Drug Administration (FDA) due to choking events and choking deaths.
- Share how a transitional food item (dysphagia training jelly) is used in dysphagia treatment in Japan and how these training jellies are different from the Konjac Jelly.
1. Challenging Transitional Foods & Mixed Consistencies
 Do you remember having Jell-O after your last bout with a stomach bug? (I know you would rather not recall that!) Your doctor may have recommended to start with “clear liquids,” like Jell-O. Seems like a simple food to handle, right? Actually, NO! It is a weird texture, going from a wiggly-slippery solid to who knows what! Jell-O is just one brand. Some gelatin products may melt in the mouth, but it seems most products break apart into tiny chunks that are hard to control.
Do you remember having Jell-O after your last bout with a stomach bug? (I know you would rather not recall that!) Your doctor may have recommended to start with “clear liquids,” like Jell-O. Seems like a simple food to handle, right? Actually, NO! It is a weird texture, going from a wiggly-slippery solid to who knows what! Jell-O is just one brand. Some gelatin products may melt in the mouth, but it seems most products break apart into tiny chunks that are hard to control.
Jell-O or gelatin may be an example of a transitional food that is potentially dangerous, as it changes from a solid into another texture or consistency. I will be using the term “Jell-O” (which is actually the brand name from Kraft Foods) to refer to all typical gelatin products found in North America. Gelatin comes from a protein collagen extracted by boiling the bones and other byproducts of the meat industry (i.e., animal hides and skins, but not hooves). Of course, a lot of sugar, flavorings and food coloring are added.
Popsicles are another example of a transitional food, as you bite off a piece and then it melts in the mouth to a thin liquid. Transitional foods are more challenging for people with difficulty swallowing, especially if they have difficulty controlling liquids and mixed consistencies in the mouth and throat. (A mixed consistency is when you have solid pieces plus liquid in the same bite, like cold cereal in milk – See this DysphagiaCafe.com article called “Mixed Consistency Dysphagia.”) While you are chewing or processing the solid food in your mouth, the liquid may be falling out of the back of your mouth and dripping down into your throat. Watermelon is another good example of a mixed consistency. Next time you chew a juicy watermelon, pay attention to the amount of liquid that cascades to the throat. Do you feel this? Do you respond quickly with a clearing swallow? If not, you could aspirate on that liquid.
If a person with dysphagia has been found to have difficulty with mixed consistencies during an instrumental swallow study, they will also likely have difficulty with bolus control in general. Bolus control is the act of keeping the liquid, food, or pill in the mouth while collecting it or managing it before starting the swallow. We can assume that Jell-O requires adequate bolus control. The solid to liquid or solid to small pieces transformations that happen with Jell-O makes it a unique and challenging transitional food item. It can become an even more challenging mixed consistency with the addition of fruit chunks.
The most challenging characteristic of most Jell-Os, per our United States IDDSI Reference Group testing was when it fractured into small chunks when the Fork Pressure Test was applied. When eating it, it fractures in the mouth, rather than forming a cohesive bolus (ball of food in the mouth). If the person with dysphagia does not have good bolus control, then the chunks of unmelted Jell-O may immediately fall to the pharynx (throat) before the swallow. This Jell-O bolus may drop to the pharynx whole or the Jell-O may fracture into particles and fall to the pharynx. Any bolus that falls to the pharynx before someone is ready to swallow (i.e., completed oral preparatory phase and volitionally move the bolus posteriorly to trigger the pharyngeal swallow response), could drop into the laryngeal vestibule (aka, larynx or airway) and cause choking and/or aspiration.
| Aspiration is when the liquid has entered into the voice box or larynx and drops down past the vocal cords into the trachea and lungs. Of course, aspiration can happen with saliva, food particles, liquids, reflux, pills and more. Aspiration over time, with other factors such as nasty oral hygiene and a poor immune system, can lead to an aspiration pneumonia. As I described in Part 2 of this blog, that can all happen silently (i.e., with no throat clearing, coughing or attempt to eject the liquid). |
| NOTE: Please make sure to consult with your speech-language pathologist (SLP) who is evaluating your swallowing. Depending on your specific type of difficulty swallowing (dysphagia), your SLP will customize your evaluation process and treatment plan tailored to your individual needs, wishes, and safety concerns. Thin liquids are not dangerous for all people with dysphagia. Thicker is not always better for everyone who has dysphagia. There are many factors that go into customizing a safest and least restrictive diet for you. |
2. Solutions for People with Dysphagia
So, for many people with dysphagia, we need a transitional food item for therapy that stays thick and smooth to allow time for processing of the food in the mouth and time to swallow, without it thinning down too much or crumbling into tiny pieces. Often after some types of stroke, for example, the swallow trigger is slow.
Therefore, if you have trouble with bolus control, gelatin and Jell-O may be on your AVOID list.
Unless…
You are savvy and find smart products that address the needs of people with dysphagia, such as:
the “Gelatein” line of products from Medtrition, Inc. These are clear liquid gelatins (similar animal-based gelatin ingredients) that stay thick and smooth and provide added protein. They are marketed as “appropriate” for patients who cannot tolerate thin liquids and require a thickened liquid (i.e., mildly thick/nectar thick through extremely thick/pudding thick). However, please make sure to ask your speech-language pathologist, as these appear to stay moderately to extremely thick (honey thick to pudding thick), and thicker is not always better for all. Some people can only tolerate a narrow range of mildly thick (nectar thick liquid), and cannot tolerate a thicker liquid, as the residue can build up in the throat.
(Disclosure: I have nothing to financially or non-financially disclose in mentioning this product).
You may also try out Magic Cup™ Frozen Dessert by Hormel Health Labs.
This ice cream does not thin down or change texture in the mouth and throat. It stays extremely thick (aka, IDDSI Level 4 or like the old term of a pudding thick liquid), so the same advice as above: consult with your speech-language pathologist to make sure it is not too thick for you.
(Financial disclosure: I am a dysphagia consultant for Hormel Health Labs on an as needed basis, but I do not receive any financial incentives to promote products.)
IMPORTANT NOTE REGARDING SUPPLEMENTS: It is so important to consult with your medical team, including your registered dietitian (RD), when adding any specialized supplement. Some products may contain ingredients that are not appropriate or safe for your individual needs (especially if you follow a special diet due to dialysis or diabetes, for examples).
3. The Dangers of Konjac Jelly & Jelly Cups:
The Konjac Jelly product is a good example of how the global public is not aware of the dangers of dysphagia! Many of us bloggers, clinicians, researchers and global organizations (such as www.IDDSI.org and the Dysphagia Research Society at www.dysphagiaresearch.org) work tirelessly to improve the public knowledge and patient safety. It is important for today’s global healthcare practitioner to be aware of potentially challenging foods from around the world.
That is why this section is a must-read.
Because the anatomy and physiology of swallowing are not well understood, you have products developed around the world that seem fun and tasty initially but end up being extreme choking risks. For example, in Japan, a candy was created with Konjac jelly (see other names for this product listed at the beginning of this blog, such as Konnyaku). Konjac is a common plant in Asia, which is like a potato or yam. These treats are very hard to chew and have been marketed heavily to children around the world. In Latin-American groceries you may have seen the name: “Nata de Coco Jelly,” which means a cream of coconut jelly.
The Konjac candy had been made into “mini-cups or jelly cups.” You peel off the top and can suck or squeeze the jelly into your mouth in one shot. Tipping your head back and sucking the jelly into your mouth may exacerbate the choking risk!
See this YouTuber (@Kouhei7JP) demonstrate how hard you have to pull to stretch the Konjac jelly substance. He says: “I can’t really show you how hard this is, but you get the idea. This is hard (pulling).” See his fingernails blanching white? As in the Fork Pressure Test of www.IDDSI.org, your fingernails blanch white at about 17-20 kilopascals of pressure (which is about the same pressure your tongue uses to push food against the palate and to swallow). Even with a lot of pulling, the Konjac jelly does not pull apart. Now imagine that in your airway causing a blockage.
See also this excellent description of Konjac jelly, used in cooking as a meat and seafood substitute, by the YouTuber: East Meets Kitchen. She describes it as a “rubbery, hard,” and a “firm sponge texture.” She realizes how much you have to chew to swallow it safely!
On YouTube, someone commented: “One would have to be stupid to choke or suffocate on Konnyaku.” Wrong! Anyone can choke, especially in this day-in-age when we are all multi-tasking and distracted. One laugh, one time talking with food in the mouth, or a quick movement or startle could cause food to fall or be sucked to the throat and airway before you were ready to chew and swallow carefully. Additionally, many people are at elevated risk for choking and difficulty managing foods safely, such as: infants, children, people with physical, mental, and/or emotional challenges, and the elderly. The comment obviously reflects how little public understanding there is of the complexity of safe swallowing and the challenges that people face every day when they have dysphagia.
The Food Safety Commission (FSC) of Japan created a Risk Assessment Report (FS/455/2010) in 2010 called: “Choking Accidents Caused by Foods.” That report lists sticky rice cakes (also known as Mochi) as the number one cause of choking, followed by these Konjac mini-cup jellies. They also note the dangers of steamed rice, bread and meat for adults and candy for infants. Per the FSC, the Konjac Jelly in all forms (mini-cups, candies, and sliceable blocks to be used as a meat/seafood substitute) are dangerous due to the following factors: smoothness of the surface, elasticity, hardness, and difficulty biting off a small size piece.
Fortunately, back in 2001, the FDA warned the public multiple times regarding the serious choking hazard. (Scroll down in the FDA document linked here until you see the section on Konjac Candy). There was a nationwide recall and eventual seizure of products from all around the United States, including in Puerto Rico. However, now with easy access to products around the world, one can buy these again. Buyer Beware!
Dysphagia specialists certainly will not be using these Konjac products in therapy.
However, these mini-cups or jelly cups are very different from the dysphagia training jelly, which has been used in Japan for people with dysphagia.
4. Another Solution: What is Dysphagia Training Jelly?
To answer that question, I contacted a colleague who I met through the Dysphagia Research Society years ago: Mari Kato-Nakao, MD, MA, PhD candidate at Tohoku University School of Medicine, who works in rehabilitation at the Yokohama Brain and Spine Center. She helped me understand Japanese dysphagia training jelly. She noted:
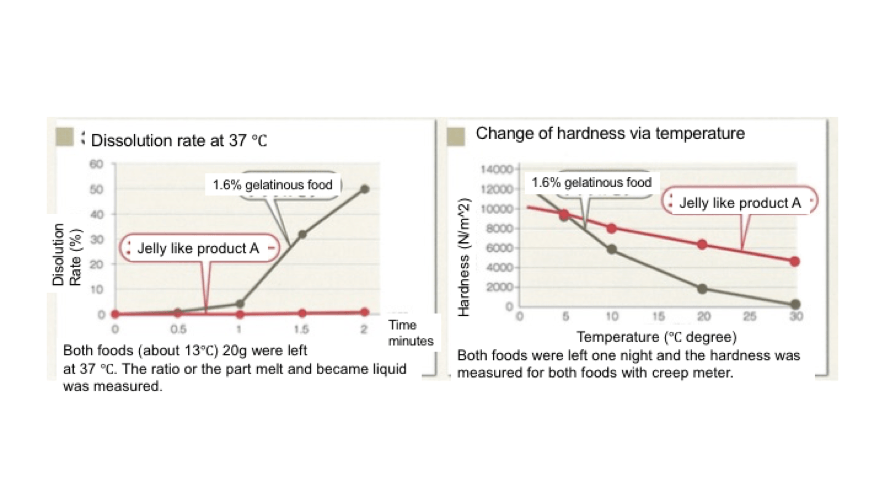
“As noted above in this blog, “normal jelly” in Japan (which is known as “Jell-O” or gelatin in the US), has a weak point to facilitate swallowing training. Pure gelatinous food can change its form into liquid with body temperature (50% dissolution in 2 min with 1.6% gelatin). This transformation loses hardness and cohesiveness quickly. Therefore, in Japan, when we feel it is not appropriate to give the patient normal gelatin or jelly which dissolves to a thin liquid, there are several jelly-like products that maintain hardness, thickness and cohesiveness in the presence of body temperature. These jelly-like products use xanthan gum, locust bean gum, carrageenan, guar gum and/or agar as gelling agents. These ingredients are what prevent the product from dissolving into a thin liquid. For clarification in this article, we are referring to these products collectively as dysphagia training jellies. See Figure 1, which is from the product information for Engelead from Otsuka.
Figure 1: Example of data from jelly-like product (product A) which is used as a sliced jelly to start swallowing exercise for NPO status. We will call this “jelly-like product” a dysphagia training jelly.
Why jelly? Clinician from other countries may wonder.
In Japan, there has been a long history of using this training jelly for dysphagia patients to train safe and effective swallowing in treatment. As you know, the International Dysphagia Diet Standardisation Initiative (IDDSI) borrowed the pyramid idea from the way Japan has depicted the standardized diets for years. Normal jellies (aka, gelatin or Jell-O) and dysphagia training jelly are within the transitional-foods category, as they start as a solid and change. However, the dysphagia training jelly does NOT dissolve all the way to a thin liquid and may be safer than other drastically changing transitional food items. In the Modified Food Pyramid from the Japanese Society of Dysphagia Rehabilitation (JSDR), jelly is situated as the easiest food with which to start. According to the previous general Japanese food pyramid, jelly was also situated in level 1 and 2, which is appropriate to start training before a purée texture.
Why is the texture easier? It is slippery and does NOT stick on the tongue when a person with dysphagia has limited ability to propel a food bolus posteriorly. This can make the texture of dysphagia training jelly suitable for people with poor tongue strength and control and poor oral coordination. Dysphagia training jelly is easy to form into bolus and does not separate into a liquid plus a solid (i.e., a more dangerous mixed consistency) before it is swallowed. We use sliced pieces of jelly for patients when upgrading people after a nil per os or nothing-by-mouth (NPO status). We consider it as the easiest food item to form a bolus. Research shows that the training jelly causes less aspiration than thickened liquids (e.g., mildly thick liquid/nectar thick or moderately thick liquid/honey thick or IDDSI levels 2 and 3, respectively) (Moriwaki, 2017).
Sakai and Kayashita (2006) reported that the appropriate food form to start with after NPO status was:
- less than 200J/m^3 as per stickiness,
- from 0.2 to 0.5 as per cohesiveness, and
- from 2000 to 7000 N/m^2 as per hardness in their research.
Dysphagia training jelly is included in this food form.
For people with Parkinson Disease (PD) and Degenerative Cerebellar Ataxia, who have poor coordination of oral phase, as well as an impaired pharyngeal phase, changing the food form into jelly was as effective as chin down posture and supraglottic swallow technique to overcome aspiration (Nagaya, et al., 2004). Nagaya and colleagues reported that 13 people with PD out of 25 showed aspiration on videofluoroscopy, but the aspiration was eliminated in these 13 participants after they changed the bolus into the jelly. Additionally, of their PD patients, only a few patients could perform a chin down posture, because their cervical muscles were too rigid. Changing food form into a jelly could be an alternative modification. The team also reported 7 out of 23 people with cerebellar ataxia showed aspiration, but the aspiration was eliminated in 5 of them after changing the bolus form into jelly.
Morita (2003) compared swallowing a powdery preparation of medication (described as bitter tasting granules) versus swallowing the medication in a deglutition aid jelly. Researchers developed this jelly that “can change almost all solid (medication) preparations into gelatinous dosage form preparations,” (per the article’s abstract). Researchers studied 10 healthy adults and found improvements in participants who had the jelly. Their total oropharyngeal transit times were a mean of 13.04 seconds and oral transit times were a mean of 10.69 seconds. Additionally, they studied some hospitalized people with dysphagia and found reduced swallow delays and reduced aspiration. This deglutition aid jelly is now considered as a suitable form of medication for elderly in Japan (e.g., for Fosamax and Aricept).
People who have some types of severe dysphagia after a stroke or who have ALS (Lou Gerig’s Disease), may be too weak to transfer the bolus to the back of the mouth to trigger a swallow. After determining that it is safe by using an instrumental evaluation (e.g., endoscopic or with videofluoroscopy), we provide the dysphagia training jelly in small amounts with a small spoon in a reclined position. See the review article by Kagagya, et al. (2011), which briefly reviews this reclined position option, as well as the potential risks of using a reclined position (such as a risk for decreased alertness and increased aspiration risk for some people). We give the training jelly in the reclined position to overcome the oral deficits of weak tongue, oral discoordination and the inability to transfer the bolus from the mouth into the pharynx. This can start retraining the pharyngeal swallow and pharyngeal contraction by swallowing a “real” bolus. We believe that the reclined position has the potential to reduce aspiration, as the thick jelly bolus travels down the posterior wall of the pharynx into the esophagus (which is situated under the trachea when the person is deeply reclined). The bolus does not come up to aspirate. We may start a person with swallowing at 30 or 45 degrees (per confirmation with instrumental testing), and then work up to a 60-degree angle and more.”
Finally, please see the www.IDDSI.org Frequently Asked Questions page on Transitional Foods and Dysphagia Training Jelly. Many IDDSI Resources can be found on the IDDSI website under the resources tab, and go to my summary of IDDSI Resources here.
Summary of Transitional Foods 3-Part Series:
Now that you are all mellow on all this Jell-O and jelly talk, let’s think about the use of transitional foods in dysphagia therapy. Comment below, share product ideas, discuss transitional foods with colleagues, and encourage research in this emerging area.
This food category of transitional foods was just defined as of 2016 when the IDDSI diet framework was published. The category of transitional foods is so vast, though. It causes us to debate the word “food” even! Are popsicles and ice chips foods? IDDSI has used ice chips as an example of a transitional food because it melts from a solid to a liquid. However, we are not worried about one ice chip like we are of one bite of Jell-O!
Can some transitional foods be used to more safely train oral control, bolus formation and mastication skills to upgrade the diet off of puree? For example, can we teach mastication better with a transitional food (like a slice of dysphagia training jelly). We know they will not choke on it in our training process, as they could on a trial piece of chicken! Can dysphagia training jelly be used more effectively and safely than ice chips to stimulate swallowing in someone who is NPO with a very severe swallowing impairment? We know that prolonged periods of NPO are detrimental, causing a worsening of the swallow function (in a “use-it-or-lose-it” principle of neuroplasticity).
This blog mentioned using a deeply reclined position, which may be controversial in the US, but it is used often in Japan. Per our training in the US, clinicians tend to always recommend a full 90-degree angle for all meals and medication passes. (Sometimes an elevated side-lying position is tried.) I do cringe when I see an elderly person being fed when slumped down in bed at a 45 degree angle. We know from Langmore and colleagues’ research (1998, 2002), that being dependent on others for feeding and being bedridden do elevate a person’s aspiration pneumonia risk. However, in Japan, they have successfully been able to re-train some very severely impaired swallow by using dysphagia training jelly and a reclined position of as low at 30-degree angle, per anecdotal reports. Obviously, we need more research.
We need to always use critical thinking, analyze each person individually, and always ask yourself and the team, “what else can we do for this person?” The customized use of transitional foods and new ideas about positioning are just two good examples of personalized medicine in dysphagia management. We maintain an open mind with each individual. But before you and the patient try some wild-new idea, keep in mind patient safety and use instrumental evaluations to confirm the plan (e.g., fiberoptic endocscopic evaluation of swallowing/FEES or videofluoroscopic swallow study/VFSS, including a reclined position).
My final words to SLPs are: please document well in your evaluations and treatments, including underlying pathophysiology that makes different kinds of transitional foods either easy or hard. For example, if someone has poor bolus control and bolus containment with posterior escape of over half of the bolus, then he may want to avoid mixed consistencies and items like Jell-O. Then you may recommend products that are transitional foods that only dissolve to a thick liquid or a very slippery puree (extremely thick liquid). Your documentation should reveal your critical thinking, your testing and treatment rationales, and provide options for diets and therapy (considering the whole individual and her goals of care). Okay, that was my CYA (you know what that means) paragraph, but also the way to ensure personalized medicine throughout a continuum of care.
See Part 1 and Part 2 of this series.
*******
New Transitional Food & Gelatin Research:
Barewal, R., Shune, S., Ball, J. et al. (2021). A Comparison of Behavior of Transitional-State Foods Under Varying Oral Conditions. Dysphagia, 36, 316-324.
https://link.springer.com/article/10.1007/s00455-020-10135-w
*******
Transitional Food References & Other References:
Dovey, T.M., Aldridge, V.K. & Martin, C.I. (2013). Measuring oral sensitivity in clinical practice: A quick and reliable behavioural method. Dysphagia, 28(4), 501-510. https://doi.org/10.1007/s00455-013-9460-2
Gisel, E.G. (1991). Effect of Food Texture on the Development of Chewing of Children Between Six Months and Two Years of Age. Developmental Medicine & Child Neurology, 33, 69-79. doi:10.1111/j.1469-8749.1991.tb14786.x
Langmore, S.E, et al. (1998). Predictors of aspiration pneumonia: How important is dysphagia? Dysphagia, 13, 69-81.
Langmore, S.E, et al. (2002). Predictors of aspiration pneumonia in nursing home residents. Dysphagia, 17(4), 298-307.
References from Mari Kato-Nakao, MD, MA, PhD on Dysphagia Training Jelly & More:
Kagaya, H., Inamoto, Y., Okada, S. & Saitoh, E. (2011). Body positions and functional training to reduce aspiration in patients with dysphagia. Japan Medical Association Journal, 54(1), 35-38.
Moriwaki, M. (2017). Engezoueikensa no Shokuhinkeitai ni okeru, Shinnyu/Goen to Intozanryu no chigai (Aspiration, penetration and pharyngeal residue depending on bolus form with videofluorography examination). Enge Igaku, 6(2), 196 – 201 [Japanese].
Sakai, M. & Kayashita, J. (2006). Physical properties of dysphagia patient. Nihon Bio and Rheoligy Gakkai Shi, 20(2), 10 – 19. [Japanese] [Abstract in English]
Morita, T. (2003). Development of deglutition aid jelly for oral administration. Yakugaku Zasshi, 123(8), 665 – 671[Japanese]. https://www.ncbi.nlm.nih.gov/pubmed/12931662 (English abstract and other references about Jelly preparations for medications, when clicking on the “J-Stage Free” tab in PubMed).
Nagaya, M., Kachi, T., Yamada, T. et al. (2004). Videofluoroscopic observations on swallowing in patients with dysphagia due to neurodegenerative diseases. Nagoya J. Med Sci., 67, 17 – 23. https://www.ncbi.nlm.nih.gov/pubmed/15279064






Comment from Facebook from Dr Catriona Steele:
When I was recently in Japan, I had a chance to visit the practice of Dr. Ken Inohara, a dentist in Fukuyama whose practice includes a teaching kitchen where patients and families are given instruction in meal preparation. Dr. Inohara had previously spent time in Canada and we found ourselves in an interesting conversation about the difference between Japanese “pudding” and Canadian “pudding”. Dr. Inohara happened to have examples of both on hand – a snack pack of vanilla pudding cups from North America and a pre-prepared Japanese pudding. For want of better descriptors, the North American pudding was thicker and more custard-like but the Japanese pudding was like “creme caramel” and very similar to flan or pudim in South America. It was more slippery than North American pudding and did not coat the spoon.
My comments in response:
Thank you Dr Catriona Steele for your comment. It is so important for us to have a thorough understanding of textures of foods from around the world – living in the beautifully globally diverse societies that we do. We need to have in depth conversations with our patients and families to really understand what their typical textures are. I love the idea of taking patients and families into a test kitchen.
Imagine a family member saying that a favorite food was a “rice cake,” and us imagining our crispy rice cakes. They are actually describing a stretchy/gummy and potentially chokable item of a sticky rice cake or a “mochi.” You mention flan, but this sometimes has a harder/slippery texture and not smooth texture. Flan may be more like custard, but our pudding should be thick and smooth. Imagine Créme Brûlée, with that hard (yummy) candy coating). Well, this is why IDDSI cannot make a perfect little diet chart of what foods go into a diet level and what foods to avoid. So much variability, even within one country!
Hi, may I know that data and graph for the Figure 1 is obtained from which paper? I already check the references but none of them cointain the graph as shown. Thank you.
That figure was from my SLP colleague in Japan. Not an article, but it was product information.
I am an SLP and I tried Cozy Pack smart Gels
This product has Locust Bean Gum- which is a thickener.
It didn’t feel to change thickness in my mouth when manipulating/swallowing.
Would this Cozy Pack smart Gel be ok for ppl on thickened liquids?
Looking for variety for snacks!
Many thanks
Mallory
I didn’t know about these before, so thanks for bringing them up.
I see that Land O Lakes has these KozyShack Smart Gels. These may be similar to the gels from Prosource Gelatein Plus that I mentioned.
However, what makes it difficult is that Land O Lakes has not done viscosity testing or labeling of what the viscosity is.
I am not sure if these Smart Gels change consistency in the mouth with heat of oral cavity. Are they feeling like a mixed consistency or transitional food item, where they start as a solid and change to a liquid? Does it melt down all the way to a thin or slightly thick level?
I will contact the company. That would be interesting to see if they have thought about usage for people on thickened liquids.
Because it has a gum-based thickener in it, I wouldn’t be surprised if it did maintain some thickness.
We will have to see.
Keep testing and questioning. That is great.
Play with it more and let me know,
Karen