Difficulty Swallowing Pills?
Learn REAL Strategies to Help You Swallow Your Pills Easily!
by Karen Sheffler, MS, CCC-SLP, BCS-S of SwallowStudy.com
Introduction to People’s Troubles with Swallowing Pills:
When I work with people who have trouble swallowing pills or fear of swallowing whole pills, I hear a lot of detailed descriptions on how hard it can be, such as:
- “I have to swallow that horse pill?”
- “I didn’t take my antibiotic pill this morning because I couldn’t swallow it.”
- “When I take pills whole with water, I choke on the pill and the liquid is probably going down the wrong way.”
- “I am afraid of swallowing pills whole; they don’t even get out of my mouth.”
- “I have to lay back at a 45-degree angle or toss my head way back to get the pill out of my mouth.”
- “I have to push the pill to the back of my mouth before I take a sip of water, to make sure the pill gets out of my mouth. Sometimes that makes me gag!”
- “My mouth is too dry, and pills get stuck on my tongue.”
- “When I first wake up in the morning, I am so stiff because of my Parkinson’s Disease, that even swallowing my Parkinson medication (which helps me get moving) is almost impossible.”
I could go on and on about both the physiological and structural reasons that people have trouble swallowing pills, but there are also many people (children, adolescents and adults) who have a real fear of swallowing pills. They may have trouble volitionally sending the pill out of the mouth due to hesitations caused by the fear of swallowing. My twelve-year-old still takes chewable tablets and liquid medications, as he cannot yet imagine the task. He has never had a negative experience swallowing a whole pill with water, but many people have had a feeling of choking and never try it again. I have worked with older adults who avoid whole pills because they vividly remember “that one time” when they were young.
People may also have trouble swallowing pills due to structural abnormalities or physiological problems causing a weak, slow, or discoordinated swallow. There are many different signs and causes of difficulty swallowing (dysphagia). Dysphagia is not a disease in-and-of-itself. Dysphagia is a symptom of a variety of different diseases, disorders, congenital abnormalities, structural abnormalities, and more, that cause difficulty swallowing. For example, dysphagia can be caused by:
- obstructive tumors of head and neck (and potentially made worse by the subsequent chemoradiation treatments);
- stroke or head injury;
- any head, neck or spinal surgeries;
- neurological diseases like Lou Gehrig’s Disease (ALS), Parkinson’s Disease, Multiple Sclerosis, Dementia/Alzheimer’s;
- swelling from intubations;
- side-effects of medications; or even
- due to a long hospitalization that caused generalized weakness.
That just names a few causes.
See this Nativ-Zeltzer & colleagues 2019 open access article link for a great summary of pill dysphagia (difficulty swallowing pills). This research article discusses the validation of a rating scale called PILL-5, which is 5 questions to help people describe and quantify their severity of difficulty swallowing pills.
Note: This scale from the same team who created the EAT-10 Scale, which helps people quantify the physical and emotional impact that difficulty eating and swallowing pills, foods, liquids has on their lives (Belafsky, et al., 2008).
For some people with dysphagia, swallowing pills can be even more challenging than swallowing foods and liquids. Pills can get stuck in the natural pockets in the throat (pharynx) or in the food tube to the stomach (esophagus). You do not want pills to hang out in these places, as the pills can start breaking down and causing injury to the lining of the pharynx and/or esophagus, not to mention the fact that the medication will not be absorbed and working for you.
November 2022 Update:
Check out my Pill Dysphagia Handout from #ASHA2022. (I spoke on this topic and risks of polypharmacy at the American Speech-Language Hearing Association’s Annual Convention, New Orleans, in the virtual library).
We All Hear: “Take Your Pills as Directed.”
That may not be so easy!
Speaking of medication absorption, there are so many things to consider to ensure you are taking your medications as directed. Your pharmacist will tell you how many times a day and when during the day to take a specific pill for best absorption, but do not forget to clarify:
Do I need to take the medication with meals or on an empty stomach?
What foods do I need to avoid when taking certain pills?
For examples:
- The following medications are typically taken on an empty stomach: Reflux medications, many thyroid medications and Sinemet (a medication that people with Parkinson’s may take that is made up of Carbidopa and Levodopa).
- Bronchodilators (e.g., Advair) require you to rinse your mouth with water, after using the inhaler, to prevent candida (aka, “thrush,” which is a fungal or yeast infection) or to prevent other mouth sores.
- To prevent pills getting stuck in the esophagus or refluxing back up when you lay down (Stoschus & Allescher, 1993; Akhtar, 2003):
-
- Take your evening medications well before laying down in bed (at least 1 hour before bed, especially if you have a large volume of pills and liquid to swallow).
- Take medications in upright position and stay upright for at least 30-60 minutes afterwards.
- Take pills with plenty of fluids, if this is safe, to prevent tissue injury from pills staying in the esophagus.
-
Those ideas may be fine if you are indeed able to easily swallow your pills with a glass of water.
However, what if that is too hard?
Strategies for Swallowing Pills:
In the past, before there were any specific products to suggest, speech-language pathologists (SLPs who specialize in swallowing) have recommended three options if a person has difficulty swallowing pills.
Please Note: Specific recommendations are dependent on the type of swallowing problem and the results of comprehensive swallowing studies. The evaluations would determine if the person was safe to take pills by mouth and provide the safest strategy for swallowing pills. See 2 case studies at the end of this blog that show images of the difficulty and the solutions.
1. Change your medications to a liquid form.
- Some people have difficulty clearing any food, pills or thick substances through the mouth, throat and/or esophagus. Sometimes the only substance that clears is a liquid. (For example, people affected by chemoradiation treatments to the neck after head/neck cancer, may have such stiffness in the swallowing mechanism that foods, purees, and even very thick liquids may not clear down.)
- However, liquid medications are not for everyone. What if you will aspirate the liquid? It would be very harmful to your lungs if liquid medications go down the wrong way.
2. Swallow them whole embedded in a smooth substance, like applesauce, yogurt, or ice cream.
- What if you aspirate ice cream? (For people at risk for aspirating thin liquids, this may not be a safe solution, as ice cream thins out when it melts in your mouth.)
- What if you are sick of applesauce? (This may be the case if you have been at the hospital or another healthcare institution for a long time.) What if you are allergic to apples?
- What if the person is confused and is spitting out the pill or holding the pill in the mouth and cheeks, while only swallowing the applesauce? (SLPs call that: “pocketing” the pill.)
- What if your medication is not absorbed as well due taking them with foods and fruit juices? (See this article by pharmacist, Dr Geraldine Moses, BPharm, DClinPharm, AACPA) .
- Additionally, see Manrique and team’s 2014 article called: Crushed Tablets: Does the administration of food vehicles and thickened fluids to aid medication swallowing alter drug release? They reviewed the literature that showed the impact of fruit juices and foods on:
- Bioavailability: what percentage of the medication is potentially absorbed by the body within 30 minutes.
- Studies have looked at the rate that medications dissolve in substances (dissolution rates). For example, Manrique and colleagues commented on research that showed how taking Dilantin (a seizure medication) in pudding may affect the bioavailability more so than in applesauce. We don’t really know the effects of all foods on all pills. This issue is made worse when we crush the pills – see below.)
- Bottom Line: Some food plus drug combinations can reduce the bioavailability of the medication in your body.
3. Crush the medications and put them in a smooth substance to swallow all at once.
- What if your pills cannot be crushed (e.g., time-release medications that need to stay whole to dissolve slowly over time)?
- What if crushing the pill and embedding it in a food causes less of the pill to be available to the body immediately (bioavailability)?
- What if you are on a thickened liquid? YOU CANNOT PUT CRUSHED PILLS INTO THICKENED LIQUIDS. The corn-starch-based thickeners and gum-based thickeners are polymers that chemically and physically bind with the crushed medications, causing a significant reduction in the dissolution rates. That means the medication itself is not fully available to your body. That is not good!
- Again, Manrique and colleagues (2014) did research on how quickly certain CRUSHED medications dissolve in liquids, foods and thickened liquids*. Even honey, jam and yogurt affected dissolution rates of some medications, like Tegretol (anti-convulsant/anti-seizure medication that is also used for nerve pain and bipolar) and Warfarin (also known as Coumadin, which helps prevent blood clots and is used often used to prevent strokes). Whereas, the honey, jam and yogurt did not affect other medications, like Norvasc and Atenolol (medications for high blood pressure and chest pain). Please also see Manrique and team’s 2016 work with Tylenol (see reference list below).
*Thickened liquids had the greatest impact on the rate that the medications were able to dissolve in comparison to water, juice, or in food items. For example, when Tegretol was crushed and placed in an extremely thick liquid/pudding thick liquid, only 14% of it dissolved in 30 minutes – that means much less bioavailability to your body.
Read more:
See Dr Julie AY Cichero’s article: Thickening agents used for dysphagia management: Effect on bioavailability of water, medication and feelings of satiety. https://nutritionj.biomedcentral.com/articles/10.1186/1475-2891-12-54
See my prior blog: Hard Pill to Swallow.
See 3D Printed Pharmaceuticals blog for a look into the future!
What Do People Need for Swallowing Pills?
We Need Better Solutions.
According to research by Carnaby-Mann & Crary (2005), people prefer an orally disintegrating tablet, as they require less effort to swallow than regular whole tablets. However, not all medications are available in this formulation (e.g., RapiTab by Schwarz Pharma, Inc). Even easier will be 3D printed pharmaceuticals that dissolve in the mouth faster even than the RapiTab technology. Aprecia, The 3DP Pharmaceutical Company is working to make this a reality, and they already have some medications in a 3D printed form. The future is bright.
For now, we need a substance that adheres to the pill or pill particles to aid in swallowing them.
BUT, this substance cannot interfere with the medications bioavailability (amount of the medication that is absorbed by the body within 30 minutes). Note: The FDA recommendation is for medication to be 85% dissolved in 30 minutes (Guidance for Industry by the US Food and Drug Administration, 1997).
The gel substance should form a cohesive ball around the pills, without affecting the pills’ ability to dissolve and be absorbed by the body quickly. A slippery gel may help to safely slide pills out of the mouth, down the throat, through the esophagus and into the stomach. Since you cannot crush medications and put them in corn starch, xanthan gum, or guar gum, this substance needs to be made from a food-grade gel that is a thick and slippery vehicle for easier swallowing.
That is why Phazix have been brought to the USA
(Update 2021: The company no longer uses the brand name: Assure Slide. They have rebranded this same product to: Phazix Pill Swallowing Gel for Professional Use, in IDDSI Levels 3 and 4. Edits made June 2021.)
Here in the USA, two brands had been introduced: Assure Slide and Phazix. “Assure Slide”(link takes you to the Array site) was the product for long-term healthcare facilities and “Phazix” was the product name for hospitals and individual consumers. Now the company is using the brand name of Phazix for all. The same product has been used in Europe and Australia for years and is labeled as Gloup. While reading this, please keep in mind that Gloup, Assure Slide and Phazix are the same product with differences only in the names, the thickness options and the flavors available.
Phazix is made from maltodextrin and seaweed extract (a type of carrageenan that is not a gum-based substance, per the company). These ingredients thicken and make a smooth gel that strongly holds the medications to help them clear through the mouth to the stomach. Phazix comes in a moderately thick/Level 3 consistency (per IDDSI.org framework standards, which is the old term of “honey thick” liquid consistency) and in an extremely thick/Level 4 consistency (aka, old term of “pudding thick” or “spoon thick” liquid consistency).
Testing by Malouh, et al. (2018) in Australia confirmed that the fruit flavored “Gloup” products were indeed moderately thick per the IDDSI Flow Tests. They also confirmed that they “Gloup Forte” passed the IDDSI testing for an extremely thick or Level 4, per IDDSI.org Framework. Malouh and colleagues noted that this product was developed to be “suitable” for people with dysphagia who need to swallow pills embedded in a vehicle or need their pills crushed and placed in a safe substance. However, this particular study only tested the actual viscosities or thicknesses and not the dissolution rates.
Research presented at a 2015 conference shows how placing crushed Acetaminophen (aka, Tylenol or Paracetamol) in Gloup had good dissolution rates, as opposed to when crushed in thickened liquids (Crinò, et al., 2015 and chart below). Both whole pills and crushed pills in Gloup were almost 100% dissolved in well under 50 minutes. See chart below showing testing of whole and crushed Acetaminophen/Tylenol in Gloup (on the left) and in water and thickened liquids (on the right). This research was presented at the Australasian Pharmaceutical Science Association (APSA) conference by Lucia Crinó and team (2015) from The University of Queensland, Australia. (Disclosure: slide provided by Assure Slide/Phazix for this article.)
Please note: The FDA recommendation is for medication to be 85% dissolved in 30 minutes (Guidance for Industry by the US Food and Drug Administration, 1997).
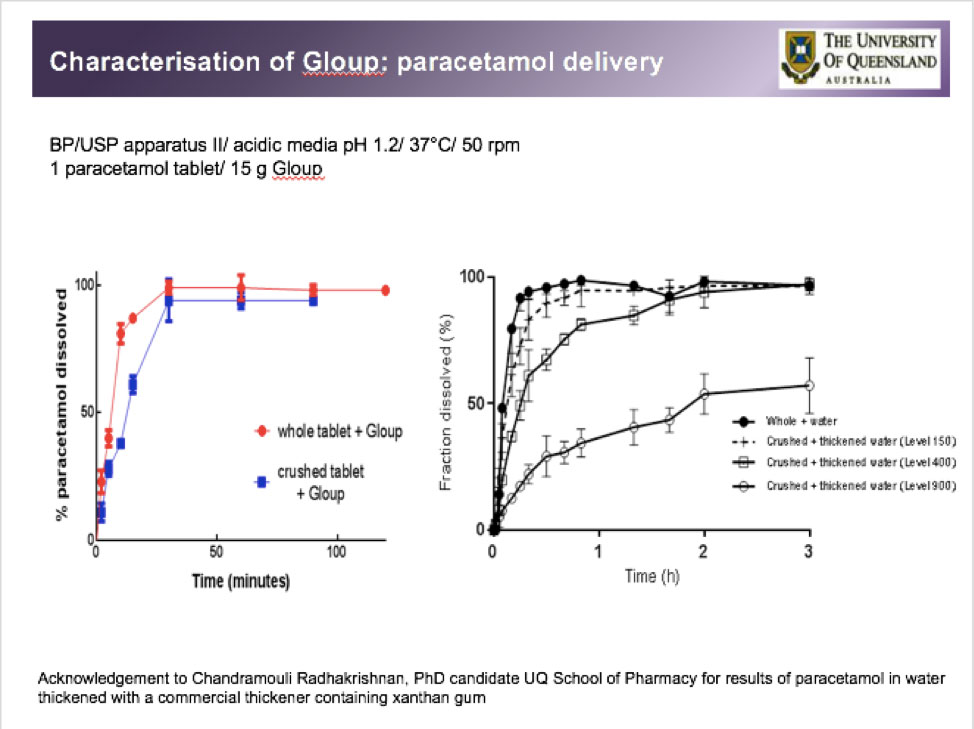
Work by the School of Pharmacy, University of Queensland, Brisbane, QLD, Australia team: Lucia Crinó, Yady J Manrique Torres, Julie A Y Cichero & Kathryn J Steadman. As noted on Slide: “Acknowledgement to Chandramouli Radhakrishnan, PhD candidate UQ School of Pharmacy for results of paracetamol in water thickened with a commercial thickener containing xanthan gum.”
Is Phazix Good for Everyone with Dysphagia?
No.
Everyone is different with different types of swallowing difficulties.
This product will not work for everyone.
As noted above, some people have difficulty swallowing moderately to extremely thick liquids (thicker liquid viscosities) due to residue getting stuck in the throat/pharynx and food tube/esophagus. These individuals may only be able to swallow thinner liquids. Everyone’s dysphagia symptoms are different.
The product does not fix the existing swallowing problem, but it may provide the perfect compensation for some. If someone’s swallow is highly impaired in safety and efficiency, even this substance can get stuck and/or be aspirated (go down the wrong way into the airway).
Therefore, it is important to view the safety and efficiency of the swallow on an instrumental examination under the guidance of a speech-language pathologist who specializes in swallowing and swallowing disorders. (Instrumental examinations are the videofluoroscopic swallow study/VFSS for viewing mouth to esophagus via x-ray or the fiberoptic endoscopic evaluation of swallow/FEES for viewing posterior oral cavity through the throat/pharynx to the top of the esophagus).
Sometimes the only way to safely administer medications is via a feeding tube or delivered through injections and intravenously. Your medical team will help guide you.
The Taste and Texture of Phazix May Help in Swallowing Pills:
Some people do not have a structural or mechanical difficulty swallowing, but they may be fearful of swallowing pills. This may even be due to a childhood choking event. They may be very hesitant to let the pill out of the mouth with liquid in order to swallow it. People who are fearful of swallowing pills tend to hold the pill in the mouth and say that they cannot swallow it. The texture and taste of Phazix may be just enough to distract the person from the fear of swallowing a pill. If the pill is “hidden” in the Phazix gel, the ball of gel can be potentially swallowed without worrying about the pill inside.
People with brain injury or dementia may “forget” how to swallow pills. Remember, the oral phase is completely under our control and requires us to “think” about sending the pill to the back of the mouth. People who are confused may spit out pills or the crushed pill pieces. If the pill is embedded in applesauce or ice cream, the person may eat the familiar food, but spit out the item inside. However, if the pill is hidden in a gel that tastes good and completely surrounds the pill, they may be more likely to swallow the gel – thereby accepting their medications.
Phazix Pill Swallowing Gel comes in is moderately thick and extremely thick viscosities and has a natural vanilla flavor. Importantly, Phazix only has 0.6 grams of sugar per teaspoon, per the company. This which far less than a typical applesauce, which has 1.26 grams per teaspoon. The person may only need a few teaspoons at most, so it is unlikely to be a significant concern for people with diabetes. (Phazix is gluten-free and contains citric acid.)
*******
Okay – you read through all those details!
Now let’s see Phazix in action with real people and their swallow studies.
*******
Case Histories and Videos to Understand the Difficulties in Swallowing Pills:
Case History 1:
(Note: No gender identifying pronouns used. Will use “they” as needed to indicate the person.)
Our first story is about a person who is 60+ years old with a history of lung cancer in the right upper lobe. They had lung surgery to remove the upper lobe, which occurred about 1 ½ months prior to this repeat videofluoroscopic swallow study. After the operation and due to prolonged endotracheal intubation (aka, a breathing tube going through the voice box/larynx into the trachea/airway), there was vocal cord injury, vocal cord immobility (not moving), swelling, and airway narrowing with granulation tissue below the vocal cords. Due to these airway problems in the voice box and trachea, they needed a tracheotomy tube placed in the neck below the vocal cords for breathing. (Read more about trach tubes at Dysphagiacafe.com‘s article.)
The first swallowing evaluation in the intensive care unit was a FEES examination (fiberoptic endoscopic evaluation of swallowing), which was done 19 days after surgery. They had penetration across all consistencies (i.e., ice chips, puree, nectar thick/mildly thick liquid, and thin liquids getting into the top of the voice box with the inability to clear them out due to poor sensation and a weak cough), as well as aspiration with thin liquid (liquid dropping below the vocal cords into the airway).
To briefly summarize for clinicians, this was due to decreased bolus control and containment, a delayed swallow initiation, and delayed and reduced laryngeal vestibule closure. (The laryngeal vestibule is your “voice box.” It is an area that is like a vestibule to your house with your inner locked door being your vocal cords, and this whole vestibule has to close up during the swallow to prevent material from getting down the wrong way). Therefore, there were issues of discoordination, poor timing and suspected weakness. Effective strategies: effortful swallows and follow-up dry swallows to clear the residue in the throat/pharynx. This was deemed a moderate oropharyngeal dysphagia. Due to the risk for aspiration with all consistencies, they were kept not eating (NPO), until a repeat swallow study could occur at rehab.
The repeat study was a videofluoroscopic swallow study (VFSS) at the rehabilitation center. They were advanced to regular textures, but they had to continue mildly thickened liquid (aka, nectar thick liquids) due to the persistent aspiration risk. Fortunately, the tracheostomy tube was removed at rehab, which was about 2 weeks prior to this last VFSS as an outpatient.
Upon coming in for this outpatient VFSS, an EAT-10 scale was provided to rate the effort of swallowing and the impact on quality of life. The effort needed to swallow pills was still rated as a 2 out of 4 on the EAT-10 scale. They felt pills frequently getting stuck with the need to wash them down with a lot of liquid. The total EAT-10 rating was 12/40, showing that eating still feels stressful, there is some fear of swallowing pills, and there is still a significant impact on the pleasure of eating and drinking.
This last VFSS showed significant improvement. There was minimal oropharyngeal and esophageal dysphagia and with no aspiration. There were only small amounts of penetration, well above the level of the vocal cords, due to slight delays in swallowing, but the penetrations were ejected with completion of the swallow. This is considered within normal limits and was not considered an aspiration risk. The only time there was an elevated risk, was when trying to swallow the barium pill with thin liquids (as seen in the video above – pill is the black disc on the tongue). The patient used a potentially dangerous strategy of tossing the head back to clear the pill off the tongue. This caused the liquid to spill to the bottom of the throat and into the airway just before the swallow. One time a trace bit of liquid reached the vocal cords but was fortunately ejected out of the laryngeal vestibule/voice box with completion of the swallow.
That barium pill was spit out. Next, we embedded the pill in “Assure Slide – Zero” (Slide was the product name at that time, which was a moderately thick gel – same as Phazix). The pill (black disc) and gel (invisible on x-ray) cleared safely through the throat without getting stuck or having the risk of aspiration on thin liquids.
***
Case History 2:
Our second story is about a person who is 70+ years old with a history of multiple cerebral cavernous malformations (CMM). These were first identified 6 years prior to this outpatient videofluoroscopic swallow study (see images below). They had their first complication of bleeding 5 years ago with the need for a resection (right craniotomy).
Note: CMM are collections of abnormally formed and enlarged capillaries with thin walls that can vary in size but are prone to leaking or causing brain bleeding.
They started having new leaking six months prior. In those 6 months, there was a challenging course of hospitalizations, rehabilitation stays, followed by visiting nurse association follow-ups, and then this repeat VFSS. Complications from the multiple brain bleeds were: confusion, dizziness, headaches, blurry vision, and unsteady gait/difficulty walking. MRIs over the hospital course confirmed multiple bilateral intracranial hemorrhages.
Two months prior, this person was found unresponsive and had aspiration on vomit. That lead to a few days of intubation (a breathing tube through the vocal cords). There was a prolonged intensive care stay. They also had increased agitation, paranoia, confusion and delirium (which can be common during intensive care stays). They received an antipsychotic medication called Haldol after extubation, which may have further caused exacerbated his difficulty swallowing. The dysphagia was likely due to the combination of bilateral neurological insults, significant mental status changes/confusion, intubation, medications, generalized weakness and de-conditioning of the muscles. Several days after extubation and the discontinuation of Haldol, they were evaluated with the first videofluoroscopic swallow study. A cautious start to eating by mouth was with a pureed diet (blended foods) and mildly thick liquids (aka, old term of “nectar” thick liquids).
During the rehabilitation stay, the liquid was changed to moderately thick liquids (aka, old term of “honey” thick liquids) during the next month, potentially due to noted difficulty with the thinner liquid (mildly thick/nectar thick liquid).
Once home (over one month and a half prior to this repeat VFSS), they were followed by an SLP and slowly upgraded to moist and soft solids (“Soft & Bite-Sized” per IDDSI.org Framework, but they were also having some soft breads, French toast, scrambled eggs, tuna fish). They remained on mildly thick liquids (nectar thick liquids) until this repeat VFSS. They have been trying thin liquids at home, but the spouse noted increased congestion and wheezing since these trials of thin liquid. There had been significant weight loss, feelings of food and pills stuck, significant coughing with meals, and an overall significant impact to quality of life. The spouse reported that they miss going out for meals.
Regarding swallowing pills, they noted that swallowing pills had been effortful, rating the severity of effort to swallow pills as a 2 out of 4 on the EAT-10 scale. They have been embedding them in applesauce, but the spouse worried that pills may still be getting stuck, especially since there are 5 pills in the morning and 10 pills at night to take.
During the VFSS, the barium pill was embedded in applesauce. We first see the pill getting stuck in the throat in a space called the valleculae (“pocket” between the base of the tongue and the epiglottis – in the throat/pharynx). When dry effortful swallows were not working, we tried a liquid wash. Washing pills down with liquid can be dangerous, causing aspiration on the liquid or pill, and this particular individual had a tendency to tip the head back. Therefore, we tried a small sip and chin tuck, which worked to clear the pill plus liquid out of the throat/pharynx without aspiration. However, then the pill got held-up in the food tube/esophagus.
In this next video, we see the pill embedded in “Assure Slide – Forte” (Slide was the product name at that time, which was an extremely thick gel – same as Phazix). It all clears easily out of the mouth and smoothly through the throat without getting stuck this time. It even pushes the other pill down through the esophagus with no further hold-up (no further esophageal retention). Both pills were emptying through the esophagus quickly.
We will not go into all the details of the videofluoroscopic swallow study here, but there was significant improvement since the last study 2 months prior. There was still a mild oropharyngeal dysphagia with safety and efficiency issues. The recommendations were to upgrade to Regular diet/Level 7 Easy to Chew (per IDDSI Framework), avoiding dry/hard/crumbly textures and foods that could elevate a choking risk (e.g., tough meats and breads). An effortful swallow was effective for more challenging foods. They were upgraded to thin/regular liquids with the caution of small single sips by cup with a chin tuck. The person was quite good at the supraglottic swallow strategy (i.e., breath hold, swallow, release breath with a cough, and reswallow). After further practice with that strategy, they could drop the use of the chin tuck maneuver. Due to the pills getting stuck in the both the pharynx and esophagus, we recommended pills to be embedded in a pill swallowing gel (Phazix). We also recommended good oral hygiene to help with aspiration pneumonia prevention, as well as pulmonary clearance exercises in case of trace aspirations of thin liquid.
*******
Financial Disclosure: Arkray USA Inc./Phazix hired this author (Karen Sheffler, MS, CCC-SLP, BCS-S) as a dysphagia consultant, and paid a small consultant fee to research and review this product. Author does not make any commission on the individual sales of the product. In June 2021, the company paid an honorarium to provide a webinar.
Update & Edits made in June 2021: The company no longer uses the brand name: Assure Slide. They have rebranded this same product to: Phazix Pill Swallowing Gel for Professional Use, in IDDSI Levels 3 and 4.
*******
November 2022 Update:
Check out my Pill Dysphagia Handout from #ASHA2022. (I spoke on this topic and risks of polypharmacy at the American Speech-Language Hearing Association’s Annual Convention, New Orleans, in the virtual library. This handout has many references and resources!)
References
Akhtar, A.J. (2003). Oral medications-induced esophageal injury in elderly patients. The American Journal of the Medical Sciences, 326(3), 133-135. https://doi.org/10.1097/00000441-200309000-00005
Belafsky, P.C., Mouadeb, D.A., Rees C.J., Pryor, J.C., Postma, G.N., Allen, J., & Leonard, R.J. (2008). Validity and reliability of the Eating Assessment Tool (EAT-10). Ann Otol Rhinol Laryngol, 117, 919-924.
Carnaby-Mann, G. & Crary, M. (2005). Pill swallowing by adults with dysphagia. Archives Otolaryngology Head and Neck Surgery, 131(11), 970-975. https://www.ncbi.nlm.nih.gov/pubmed/16301368
Cichero, J.A.Y. (2013). Thickened agents used for dysphagia management: Effect on bioavailability of water, medication and feelings of satiety. Nutrition Journal, 12, 54. https://nutritionj.biomedcentral.com/articles/10.1186/1475-2891-12-54
Crinò, L., Manrique Torres, Y.J., Cichero, J.A.Y. & Steadman, K.J. (2015, November-December). Characterisation of Gloup: Is it suitable for medication delivery in dysphagic patients? Session presented at Australian Pharmaceutical Association (APSA) Annual Conference, Hobart, Tasmania, Australia.
Guidance for Industry. Dissolution testing of immediate release solid oral dosage forms. United States Food and Drug Administration, Rockville, MD, 1997.
Malouh, M.A., Cichero, J.A.Y, Manrique, Y.J., Crinò, L., and Steadman, K.J. (2018, December). Helping patients to swallow their tablets: Is Gloup appropriate for use in dysphagia? Session presented at Australian Pharmaceutical Association (APSA) Annual Conference, University of South Australia, Adelaide, Australia.
Manrique, Y.J., Lee, D.J., Islam, F., Nissen, L.M., Cichero, J.A.Y, Stokes, J.R. & Steadman, K.J. (2014). Crushed tablets: Does the administration of food vehicles and thickened fluids to aid medication swallowing alter drug release? Journal of Pharmacy and Pharmaceutical Sciences, 17(2), 207-219.
Nativ-Zeltzer, N., Bayoumi, A., Mandin, V. P., Kaufman, M., Seeni, I., Kuhn, M. A., & Belafsky, P. C. (2019). Validation of the PILL-5: A 5-Item Patient Reported Outcome Measure for Pill Dysphagia. Frontiers in surgery, 6, 43. doi:10.3389/fsurg.2019.00043 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6667828
Stroschus, B., & Allescher, H.D. (1993). Drug-induced dysphagia. Dysphagia, 8, 154-159.



Hi. I know this post is more than 6 months old now so I don’t know if you’re monitoring comments but I wonder if you can shed light on something that I haven’t been able to research.
In the morning, I take a total of 9 pills (I then take 3 in the afternoon and 4 in the evening). Ordinarily I have no problem swallowing pills at all – my gag refex is practically non-existent and I can dry-swallow even the very large circular pills if I had to (I don’t do that, I just CAN).
But the weird thing is, after I take ohhhh 5 pills or so, it becomes very difficult to take any more. It doesn’t activate my gag reflex or anything – the pills just won’t go down when I swallow, instead hanging around at the opening to my throat. It really has to be forced with a concerted effort and lot of liquid, which often leaves me feeling slightly nauseated by the time I get all 10 in my system. There are no issues with the afternoon and evening doses of the same pills.
I ONLY get this problem if I have to take a lot of pills at once – it’s like my body just “gives up” on the whole thing after a while and though the liquid goes down fine the tablets are just left behind.
Do you have any insight into why that happens/whether I can do anything about it?
Of course any impressions/advice I suggest here should be reviewed with your medical team before any action is taken or not taken.
I wonder if your pills start getting hung up in the esophagus (food tube to the stomach). Point to where on yourself that they feel stuck. Are you pointing to that notch area at your lower throat? That may indicate that pills are getting hung up in the esophagus and not clearing quickly through the esophagus as they had when you were maybe younger. Squeezing action of our esophagus can get sluggish as we get older. Then I wonder if the issue is worse in the morning specifically because you may have some issues of reflux at night. Reflux can irritate the lining at the bottom of the esophagus and may make it more swollen in the morning. By afternoon and evening, are you already on your doses of your anti-reflux medication? You could also see the blog I have on reflux (Search: So I was told I have reflux: What next?)
To figure out why this is happening, consider a barium swallow/timed barium swallow study at your local hospital with the radiology department, asking for testing a barium pill too.
If you have significant reflux and maybe pain with it too, then you could consider a GI endoscopy to scope your esophagus with a camera and see if there is irritation to the lining of the esophagus. Structural narrowing that causes pills to get stuck? Do you also feel steak and bread get stuck after several bites?
You could try reflux precautions like head of bed elevation at night.
You could also try taking the pills embedded in a substance that is slippery like what I mentioned in this blog. (I don’t receive any kickbacks or financial gains on suggesting that). That may help in not filling up on a ton of water in an effort to push down a pill. Often during our videoswallow studies, we see a pill sit there when the liquid just washes past it.
Best of luck and please keep us posted! Your comments will I’m sure help others.
Great analysis, I love how you really went in-depth with everything it really projects what one needs to know about trouble swallowing pills what to do for pill dysphagia. You have done an excellent job with this content I must say.This resource Gembrahealth.com i came across recently and is nice too as this particular site.
Help me with my swallow am losing weight I can’t eat take drugs am suffering of swallow please help me
Hello Mariam,
Swallowing disorders are very complex and multifactorial (caused by many different issues). The best way to begin comprehensive evaluation and treatment is to find a speech-language pathologist who specializes in swallowing. To find a board certified specialist, consider going to http://www.swallowingdisorders.org – which is the American Board of Swallowing and Swallowing Disorders. Here is their “find an specialist” page. You can enter in your state and find a list of specialists: https://www.swallowingdisorders.org/search/custom.asp?id=1177
To see a speech language pathologist (SLP), you would need to discuss your symptoms with your primary care doctor to get an order and a referral. The SLP will start with a thorough interview and evaluation. Likely, you would need an evaluation that shows us inside your swallow. See these blogs:
How do I know I need a swallow study?
How is my swallow evaluated: SwallowStudy.com for Dysphagia
You may also ask your doctor for a referral to see a dietitian (registered dietitian nutritionist / RDN) who can further address eating and weight loss issue. It is important to advocate for yourself and seek out these specialists.
Here is the “find a specialist” page from the Academy of Nutrition and Dietetics: https://www.eatright.org/find-a-nutrition-expert
I hope that starts you on the road to recovery!
It is just so hard to try to address all the issues over communications over email or the internet.
I hope you find specialists.
Sincerely,
Karen from SwallowStudy.com
Highly descriptive blog, I enjoyed that a lot. Will there be a part 2?
Thank you!
Please also see:
Hard Pill to Swallow? Pill Dysphagia
3D Printed Pharmaceuticals Summit
Think Outside the (Pill) Box: 3D Printed Pharmaceuticals
Drug-Induced Dysphagia Resources & Safe Practices
Please let me know if you have questions.