Pneumonia Alphabet Soup (Part 2): The Secret Ingredients
by Karen Sheffler, MS, CCC-SLP, BCS-S of SwallowStudy.com (Parts 1 & 2 first published by MedbridgeEducation.com)
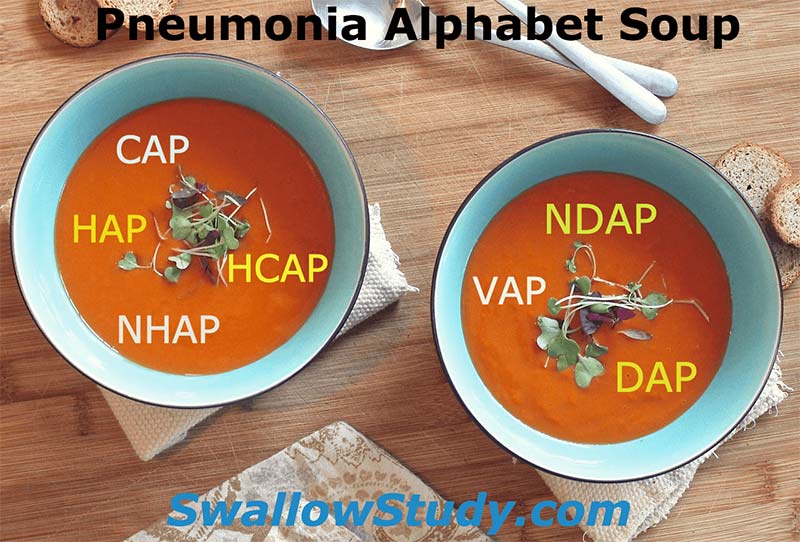
We began deciphering the recipe of pneumonia in Part 1 – Pneumonia Alphabet Soup: Reworking the Recipes. I suggested that it is more important to think about how the pneumonia was acquired, rather than where it was acquired [i.e., community-acquired pneumonia (CAP), health-care-associated pneumonia (HCAP)]. Causes for pneumonia are multifactoral, and the clinician may have to consider the following factors:
-
Pneumonia risk factors (for example, dependency on others to feed and to perform good oral care),
-
Patient’s functional baseline status before getting sick, and
-
Events that lead up to the onset of the acute illness.
Taking a holistic approach to diagnosis and treatment can help the medical team see all the potential ingredients of the “pneumonia soup.” If a multifactoral-aspiration pneumonia is suspected, there is still work to be done to uncover the secret ingredients.
Ask More Questions About the Pneumonia:
1. Was the pneumonia a sudden onset within acute care?
Pneumonia acquired in acute care may be caused by a sudden aspiration event, dysphagia caused by the weakness and acuity of the illness, or an iatrogenic cause. (Iatrogenic means an unintended adverse complication or side effect of medications, treatment, or invasive procedures, like surgery or intubation.) Ask, did the person re-start eating and drinking too soon?
In a 1998 study, Langmore and colleagues separately analyzed acute care subjects to determine their specific factors associated with pneumonia. While the number of decayed teeth and dependence for oral care remained significant, they also found that dysphagia and aspiration were strongly associated with pneumonia (4). Specifically, the following are the dysphagia and aspiration risk factors:
-
aspiration of food,
-
pharyngeal delay,
-
low spillage point for the bolus during a delay (i.e., spillage to pyriforms), and
-
excess residue post-swallow
Patients at risk for aspiration have higher rates of 1-year mortality, readmissions, recurrence of pneumonia, and development of gram-negative bacteria (7). The following factors place patients in an aspiration risk group (1,7):
-
witnessed aspiration,
-
vomiting,
-
dysphagia confirmed by formal evaluation,
-
impaired consciousness from ETOH/drugs/medications, and
-
chronic neurologic diseases and disorders, and
-
esophageal disorders and obstructions.
The hospitalized patient, when conditions are ripe, has an elevated risk for a nosocomial infection like Hospital-Acquired Pneumonia (HAP). I like to use the term Hospital Acquired Pneumonia still, as this can push hospitals to perform root-cause analysis and try to prevent some of these hospital acquired infections (HAIs). These infections could potentially be prevented by establishing hospital-wide screening protocols for dysphagia and referring immediately to a speech-language pathologist (SLP) for a full bedside swallowing evaluation upon failing the swallow screen.
2. Was the pneumonia a gradual onset?
With our very elderly patients from nursing facilities, we often say: “That was the straw that broke the camel’s back.” In other words, the resident may have followed a more gradual functional decline due to chronic disease, bedridden status, and dependency, leading to increased severity and frequency of aspirations along with the eventual inability to compensate (5). This patient may be admitted to the hospital with what used to be labeled as a Nursing-Home Acquired Pneumonia (NHAP) and now is termed HealthCare-Associated Pneumonia (HCAP).
3. Which came first: the aspiration, the dysphagia or the pneumonia?
To sort this out, I think the most useful labels I have seen are:
-
Dysphagia-Related Aspiration Pneumonia (DAP) and
-
Non-Dysphagia-Related Aspiration Pneumonia (NDAP).
I first heard these used by Dr James Coyle, PhD, CCC-SLP, BCS-S, of University of Pittsburgh at the ASHA Healthcare & Business Institute in 2014 (2), but the terms were also present in his 2010 article with Christine Matthews, CSCD, CCC-SLP (3).
To select the appropriate label, we need to figure out if the functional decline and the aspiration pneumonia were due to a pre-existing dysphagia or not. Coyle and Matthews used the analogy of “which came first, the chicken or the egg” with this question (3):
“Is the clinician seeing the chicken (dysphagia caused the aspiration pneumonia) or the egg (pneumonia has caused acute reversible dysphagia)? It is possible that the truth is more complex—that dysphagia has caused pneumonia that has acutely worsened pre-existing dysphagia.”
Yes, that is complex. Let’s address each potential secret ingredient individually.
Further Analysis of the Pneumonia Ingredients: 4 More Questions
1. Did the dysphagia come first?
If so, we would use the label Dysphagia-Related Aspiration Pneumonia (DAP). However, this label does not even tell the whole story.
a. What type of dysphagia?
Was it an oral dysphagia, an oropharyngeal dysphagia, an esophageal dysphagia, or all of the above? Esophageal dysphagia can be overlooked (See prior Esophageal blog). Pharyngeal and esophageal dysphagia can frequently co-occur. Langmore’s team found esophageal dysmotility to be significantly associated with pneumonia, potentially due to slow and incomplete esophageal emptying (4). Esophageal disorders and obstructions placed patients in an aspiration-risk group, as noted above in Taylor’s study (7). Esophageal dysphagia can cause esophageal backflow or retrograde flow of food/liquid to the pharynx which can enter the airway. (This aspiration may be called: laryngopharyngeal reflux/LPR, pharyngoesophageal reflux, or supraesophageal reflux – talk about too many labels!)
As stated in prior blogs on the topic of: Good Evaluations Guide Treatment, instrumental testing is the best way to assess the pathophysiology of the swallow (e.g., Fiberoptic Endoscopic Evaluation of Swallowing/FEES and/or VideoFluoroscopic SwallowStudy.com/VFSS, aka Modified Barium Swallow/MBS). The oral, pharyngeal and esophageal phases are addressed. After testing, the clinician can make appropriate recommendations and referrals (i.e., to GI if esophageal issues are suspected).
b. When did the dysphagia start?
Was it an acute or gradual onset of dysphagia? This may take careful research during your clinical bedside evaluation. It usually requires good detective work, including, but not limited to, talking at length with the patient and main caregivers, talking with staff, and calling the person’s nursing facility, rehab center or assisted living facility. Keep in mind, what gets labeled as a Community-Acquired Pneumonia (CAP) may in fact be due to chronic dysphagia. Additionally, dysphagia is not a disease in-and-of-itself, so what is/are the underlining condition(s) that caused it?
If there was no chronic baseline of dysphagia, that brings us to our next question.
2. Did a functional decline from an infection come first?
Upper respiratory infections and urinary tract infections (UTI) can cause generalized weakness, fever, lethargy, delirium, and a new bedfast state. Confusion is caused by the acute infection and can be exacerbated by medications and an unfamiliar environment with an interrupted sleep schedule. The weakness and cognitive changes may have then cause an acute onset of dysphagia, leading to an acute aspiration risk. This should be cautiously labeled a Dysphagia-Related Aspiration Pneumonia (DAP). The clinician and team has to remember that this process may have occurred in the absence of a baseline of dysphagia. Maybe the person’s baseline was independent and high functioning. However, once a person is labeled “a dysphagic aspirator,” the label may stick for far too long. The medical team may feel pressure to to be overly restrictive. Therefore, the goal should be to quickly upgrade the patient’s diet once the acute phase has resolved.
3. Did a vomiting and/or refluxing episode come first?
Aspiration pneumonitis due to aspiration of vomitus is an example of a Non-Dysphagia Related Aspiration Pneumonia (NDAP) (3).
Distinctions need to be made between aspiration pneumonia (infection caused by aspiration of material colonized by pathogens, from the oral cavity or GI tract in the presence of proton pump inhibitors) and pneumonitis (non-infectious chemical burn or lung injury causing inflammation). However, an acute inflammation can make the lung more susceptible to a subsequent infection. Aspiration pneumonitis does not have an acronym; therefore, I wonder if gets forgotten and patients get over treated with antibiotics.
That said, similarities can be found between aspiration pneumonia and aspiration pneumonitis, especially in the area of prevention:
“For both syndromes, the best strategy is prevention. Preventive measures in the preoperative period and in the chronically ill patient at high risk for aspiration must be ensured to avoid complications.” (6, p370)
4. Did the pneumonia come first?
A pneumonia may have been caused by aspiration of colonized oral pathogens along an endotracheal tube (Ventilator Acquired Pneumonia). This could be considered a Non-Dysphagia-Related Aspiration Pneumonia (NDAP).
Another example is how a severe septic state (i.e., urosepsis) can progress into a hematogenous pneumonia. This type of pneumonia should not be labeled a Non-Dysphagia-Related Aspiration Pneumonia, as it is NOT even an aspiration pneumonia.
However, it is part of our job to recognize that the subsequent lethargy, weakness, medication side-effects and intubations could then cause an acute-reversible dysphagia. (Our digging through the medical record and baseline should tell us that the patient did not have a baseline dysphagia.) However, if we recognize the acute risks and recommend initially proceeding with caution, this could prevent an additional nosocomial-multifactoral aspiration pneumonia. Once the acuity has resolved, we can advocate for re-evaluations, especially at the rehabilitation center. Again, the goal should be to return this patient to oral intake and a least restrictive diet as soon as possible.
Conclusion:
The letters in the pneumonia soup (from Part 1) float on the surface and do not necessarily point to the root cause. Ask: “Is the label useful?” We need to dig in deeper, stirring and tasting the soup to find the secret ingredients.
We not only evaluate the patient’s current cognitive, oral motor, speech-language, voice and swallowing status, but we also critically analyze the patient’s baseline functional status, past medical history, onset of current illness, and related factors that may have contributed to an increased risk for dysphagia, aspiration, and/or pneumonia. We need to ask questions to better understand the context surrounding the patient’s acute condition. We need to be careful with our impressions and recommendations. If we only emphasize the severity of the dysphagia and aspiration risk in our documentation, then the medical team may be quick to jump to NPO status and a feeding tube without considering the bigger picture. The patient may carry the aspirator label around too long and remain overly restricted.
My husband can take a spoonful of soup and guess the secret ingredients, declaring: “Ah, lemon and cardamon.” The medical team may look to the Speech-Language Pathologist to help understand the special recipe that went into the patient’s pneumonia.
For further reading, see my blog: “7 Clues in Medical Record to Discover Dysphagia”
References:
- Chalmers, J.D., Taylor, J.K., Singanayagam, A., Fleming, G.B., Akram, A.R., Mandal, P., et al., (2011). Epidemiology, Antibiotic Therapy, and Clinical outcomes in Health Care-Associated Pneumonia: A UK cohort study. Clinical Infectious Diseases, 53 (2), 107-113. doi: 10.1093/cid/cir274 https://cid.oxfordjournals.org/content/53/2/107.long
- Coyle, J.L. (2014, April). When the cause of dysphagia is not obvious: Sorting through treasure and surprises in the medical record. Session presented at ASHA Health Care & Business Institute, Las Vegas, NV.
- Coyle, J.L. & Matthews, C. (2010). A dilemma in dysphagia management: Is aspiration pneumonia the chicken or the egg? The ASHA Leader, 15, 14-17. doi:10.1044/leader.FTR2.15062010.14 https://leader.pubs.asha.org/article.aspx?articleid=2291889&resultClick=1
-
Langmore, S.E, et al. (1998). Predictors of aspiration pneumonia: How important is dysphagia? Dysphagia, 13, 69-81.
- Langmore, S.E, et al. (2002). Predictors of aspiration pneumonia in nursing home residents. Dysphagia, 17 (4), 298-307.
-
Strachan & Solomita. (2007). Aspiration syndromes: Pneumonia and pneumonitis – preventive measures are still the best strategy. The Journal of Respiratory Diseases, 28 (9), 370.
-
Taylor, J.K., Fleming, G.B., Singanayagam, A., Hill, A.T. & Chalmers, J.D. (2013). Risk factors for aspiration in community-acquired pneumonia: Analysis of a hospitalized UK cohort. The American Journal of Medicine, 126 (11), 995-1001.