Multiphase Dysphagia Evaluations: Pharyngoesophageal Inter-Relationships
by Karen Sheffler, MS, CCC-SLP, BCS-S of SwallowStudy.com
This Dysphagia Digest stresses the importance of multiphase dysphagia evaluations, and it is in honor of the Dysphagia Research Society’s (DRS) Dodds Donner Lecture. The annual lecture is in remembrance of:
- Dr Wylie Jerry Dodds, MD of the Medical College of Wisconsin
- Dr Martin W. Donner, MD, a leader at the Johns Hopkins Swallowing Center and the Hopkins Department of Radiology
Both were professors in radiology and medicine and were prolific researchers in gastrointestinal radiology, esophageal disorders and motility disorders. They were early pioneers in the field of dysphagia, and the Dysphagia Research Society and its members may not be here today if not for them.
Introduction & Inspiration
My inspiration for writing this article was DRS’s 2019 Dodds Donner lecturer: Joel Richter, MD, FACP, MACG. Dr Richter is a professor of medicine and oncologic sciences, an endowed chair of the Morsani College of Medicine, the Hugh F. Culverhouse Chair for Esophagology, the Director of the Division of Digestive Diseases and Nutrition — at the University of South Florida (USF Health) in Tampa, FL. He is also the director of the Joy McCann Culverhouse Center for Swallowing Disorders, where he works closely with speech-language pathologists (SLPs) who specialize in swallowing.
Dodds Donner Award given to Dr Joel Ritcher, MD, FACP, MACG by DRS 2018-2019 President Sudarshan R. Jadcherla, MD, DCH, FRCP (Irel), AGAF at Dysphagia Research Society 2019, San Diego, CA.
It was an honor to hear his lecture titled:
“The Patient with Dysphagia: In the Future, Who Will Take Ownership?”
He worries that no one is fully taking this ownership, but he wants to see the future “brighter and better!”
After all his experience in the field of dysphagia, he declared:
“Who else better to really lead this evaluation than the SLP.”
He acknowledged that the speech-language pathologist’s skill-set and the scope of practice put SLPs in the perfect position to perform comprehensive multiphase dysphagia evaluations. It is often very complex and multifactorial issues that make up a person’s dysphagia. SLPs can be leaders in this differential diagnosis process. We do thorough chart reviews and interviews, and from our initial evaluations and instrumental evaluations, we can help tailor the diagnostic and treatment process.
Swallowing is a Synchrony of Complex Inter-relationships – Not a Dichotomy
Swallowing “is not a dichotomous process,” he explained, as often the patient does not have only a pharyngeal (throat) issue or just an esophageal (food tube to the stomach) issue. Swallowing is a “continuous process” – all the way from the eating environment and the sensory input of the food and liquid in front of you to when the bolus (ball of food/liquid) passes through the esophagus and into the stomach. The SLP’s interview with the individual and caregivers looks at the issues holistically across many factors (e.g., feeding environment, quality of life, cognition, medications, dry mouth, reflux and globus sensations, positioning, just to name a few). During our comprehensive multiphase dysphagia evaluations, we cannot break apart the oral versus pharyngeal versus esophageal phases as they are interconnected and influenced by many factors.
Dr Jerilyn A. Logemann, in the Evaluation and Treatment of Swallowing Disorderstextbook from 1983 and in her Manual for the Videofluorographic Study of Swallowingfrom 1986 and 1993, originally simplified the study of swallowing into 4 phases: oral preparatory, oral, pharyngeal and esophageal. However, these phases are complex and crucially inter-related. Humbert and colleagues say it well with this quote from their 2012 paper:
“Models of swallowing biomechanics are typically divided into phases… These phases are physiologically interconnected but distinguishing among them helps to explain the biomechanical and neural control mechanisms associated with the swallowing process as a whole. Although discussed as separate processes, the interdependence of the phases must be considered throughout (p 204).”
Doctors often want to know if their patient has oropharyngeal OR esophageal dysphagia. It is often not so simple. Just as swallowing tests are not pass or fail, dysphagia cannot be easily put into one category or another. Dysphagia is often multi-factorial, involves multiple phases, and frequently requires multiple disciplines and tests. Richter reminded that many medical conditions have multi-phase dysphagia findings, and even our swallowing strategies can have a multi-phase impact (such as the double swallow affecting the esophageal clearing wave).
Unfortunately, medicine may have created and reinforced this dichotomy. Medical specialties (otolaryngology versus gastroenterology), as well as our testing (modified barium swallow study/MBSS, aka, videofluoroscopic swallow study/VFSS versus the barium swallow/esophagram) have for years separated oropharyngeal from esophageal issues. It should not be the SLP’s exam versus the radiologist’s exam.
All this has left Richter asking:
Who is looking at the whole swallow?
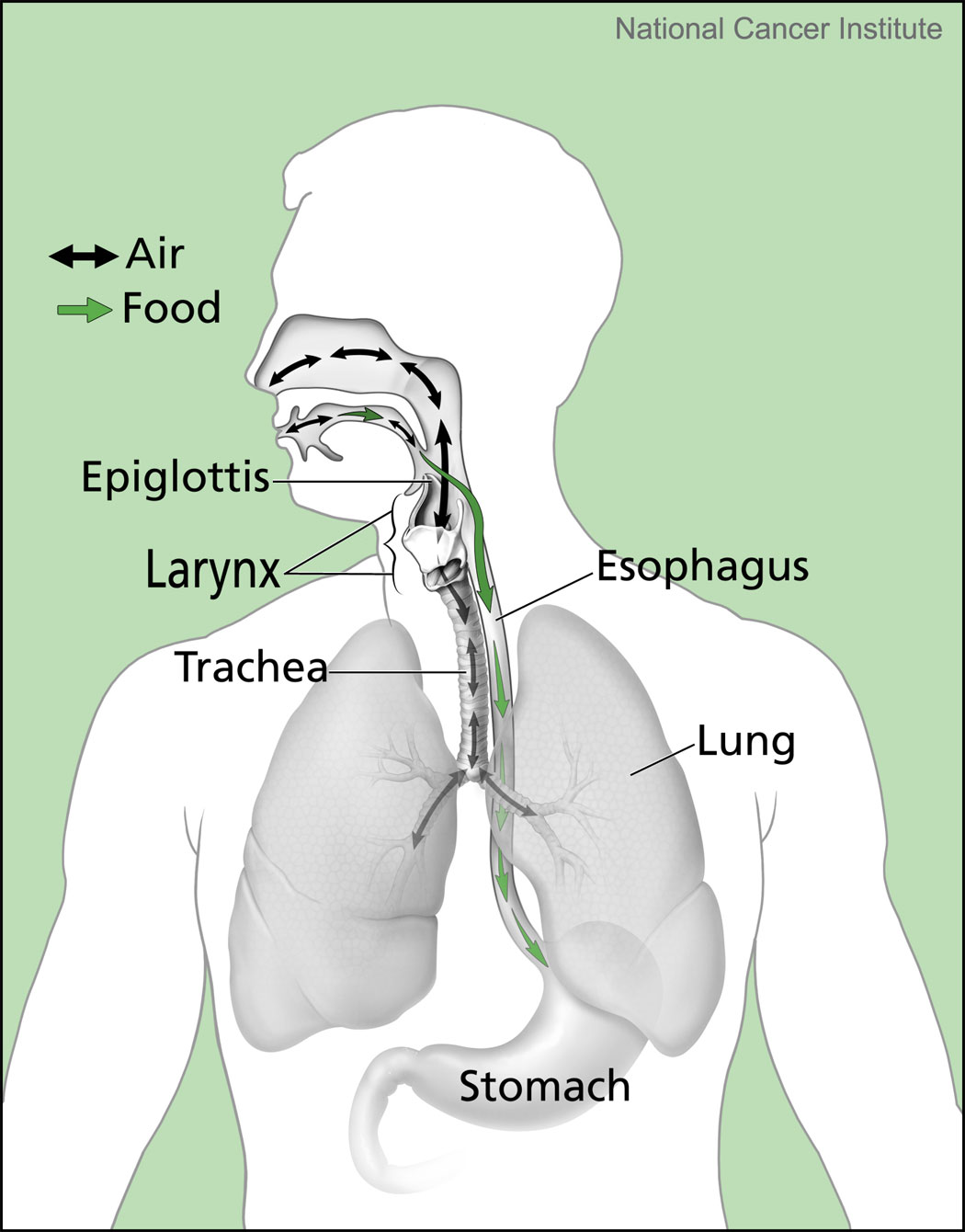
Oral, pharyngeal and esophageal inter-relationships are important to consider. SLPs perform multiphase dysphagia evaluations when looking at the safety and efficiency of food, liquid, saliva, and pills traveling to the stomach.
I recently collaborated with a radiology resident to provide a more thorough barium swallow/esophagram on a patient who was regurgitating at every meal. The radiology resident was open and appreciative. Due to that collaboration, the patient understood his severe esophageal dysmotility better. During typical barium swallow studies, the radiologist walks out of the room after the last image is taken, as the radiologist may have a plus/minus or diagnostic mindset. Who is there with the patient to do the following?
- Test swallowing strategies during the exam,
- Train the effective strategies after the exam,
- Stay in the room to explain the results (with using a translator as needed),
- Educate on the multifactorial issues that make up the dysphagia,
- Plan referral options for further testing, and
- Provide management options and eating/nutrition options (which can be discussed by the patient with the whole medical team).
Richter states:
“SLPs are well positioned to be the professionals that have a stake in comprehensive dysphagia assessment.”
Read more about esophageal dysphagia in this blog called: How Low Do You Go?

A VFSS that stops at the top of the esophagus could miss this. The SLP does not diagnose this, but the SLP does comment on bolus clearance, risks, & refers to Gastroenterology. This severely distended esophagus is filled with barium. High risk for retrograde flow, backflow into pharynx and spillover into larynx, causing aspiration after the swallow.
Diagnostic Mindset Plus a Therapeutic Mindset Needed in Multiphase Dysphagia Evaluations
This diagnostic-only mindset and potential misconceptions can be seen in the 2019 editorial article, called “To Sweep or Not to Sweep,” by Dr Olle Ekberg (prominent radiologist and professor from Lund University in Sweden). He incorrectly states that SLPs “see the esophagus as an auxiliary tube not worthy of a meticulous evaluation.” Ekberg also calls the robust esophageal sweep test and protocol proposed by Dr Joel Richter and colleagues (Watts, et al., 2019) a “superfluous cursory approach” and a “cursory view.” However, the robust esophageal sweep test (REST protocol) includes scanning the esophagus after a solid, multiple large volume sips of liquids and a pill. This is more thorough than what is done for most barium swallow studies, which do not test solids at all.
Ekberg questioned the “aim” of the comprehensive videofluoroscopic examination proposed by Watts, Richter and other colleagues (2019), saying that we should strictly separate our diagnostic goals from our therapeutic goals.
This has been a misunderstood aspect of our VFSS/MBSS studies for years. We do not have a pass/fail, plus/minus or diagnostic-only aim. If we did, we would walk out of the room as soon as the first aspiration was found. Instead, we perform thorough examinations of the safety and efficiency of the swallowing, figuring out WHY the person is having aspiration or residue. We educate people about why they are having problems and what we can do about it. We determine the underlying structural and physiological reasons for the safety and efficiency issues. We investigate the whole swallow on the VFSS from the mouth to when the bolus passes through the esophagus (as long as this is visible per positioning and body habitus constraints). We refer for further testing to help figure out more of the diagnostic aspects about why the dysphagia is happening. Figuring out why it is happening is the first part of treatment, as noted by Ekberg. However, we cannot send the person away without providing guidance on how to swallow safer and more functional in the meantime. We must have diagnosis and therapeutic aims at the same time!
Ekberg says that the diagnostic test should focuses on “explaining the patients’ symptoms,” but if we only focus on a person’s symptom of food getting stuck in the pharynx, then we may tell the person it is all in his head when nothing no food was found in the pharynx. We know the person’s sensations can be faulty (read more below in the referred sensations section). That is a disservice to the patient. We must dig deeper to make sure we are not missing something. We must perform these esophageal scans!
Ekberg concluded with “don’t rely on the cursory sweep.” We fully agree there. I would like to assure radiologists that we do not rely solely on our multiple esophageal sweeps with liquids, solids and pills. Our comprehensive multiphase dysphagia evaluation also:
- incorporates an extensive medical record review,
- gathers information from a thorough patient/caregiver interview,
- refers immediately to the appropriate specialists for further evaluations, and
- plans dysphagia therapy follow-up as needed.
Without SLP’s careful consideration of the esophagus in our holistic approach to dysphagia, many issues would go un-identified, under-evaluated and untreated. The following scenario has happened too often for me to ignore the esophagus: A patient comes to the SLP with complaints of “foods sticking in the throat,” the SLP’s careful eye on an esophageal sweep sees significant esophageal retention and an irregular mucosal lining. The SLP’s careful history-taking leads the SLP to discuss these critical findings immediately with the radiologist and medical team. The patient receives a quick referral to identify and treat an esophageal cancer.
Where Have the Artists Gone?
In Richter’s lecture, he noted that the general physicians should be skilled in “the art of good history-taking.” However, the information gathered regarding swallowing in a history and physical examination is often not thorough and can be based on myths (such as that a gag reflex can be used to predict dysphagia and aspiration risk). See more dysphagia myths below.
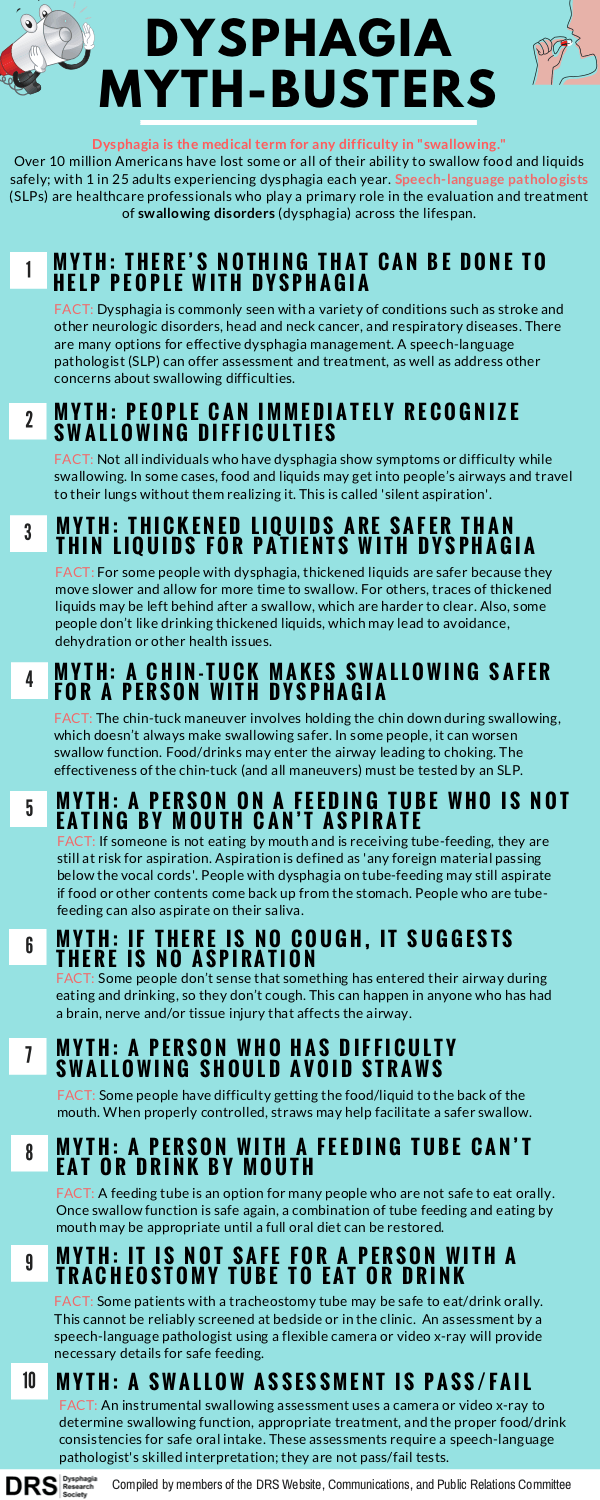
Dysphagia Myth-Busters from DRS 2018 – crucial to know when performing multiphase dysphagia evaluations, counseling patients & planning dysphagia treatment.
Richter also pointed to the 2009 article by Dr Levine and colleagues lamenting on the lost “art” of the barium swallow. Richter wonders “where have the artists gone.” The new radiologists are swept away by the high-tech and higher reimbursable CTs and MRIs. Richter noted that the barium swallow study is safe, cost-effective and highly informative when done well. Levine’s article comments on the vicious cycle created by a slow and steady decline in the amount of barium swallow studies being performed:
“As radiologists perform fewer barium studies, it has become increasingly difficult for them to maintain the fluoroscopic skills required for high-quality studies (p 19).”
I propose that the SLPs are the artists in performing comprehensive multiphase dysphagia evaluations, collaborating with the radiologist and the entire medical team to provide thorough tailored evaluations and targeted treatment. (Read more about personalized medicine in dysphagia in my article in MedbridgeEducation: Personalizing Dysphagia Evaluation: The Platinum Standard.)
The memorial article about Dr Martin Donner (Dysphagia, 1992) pointed to his art of history-taking and tailored evaluations:
“The feeding evaluation began with his careful, annotated clinical history, and the radiologic examination was tailored (a favorite word) to the person’s problem.”
Referred Sensations Make Some People’s Symptoms & Complaints Inaccurate
People are often referred to speech-language pathologists with complaints of food and liquid getting stuck. We know from research that people are not always accurate in pointing to exactly where they are having the problem. The esophagus is just not wired for detailed sensory feedback, and very often people get a referred sensation high in the neck, even when that food, pill and/or liquid is actually stuck at the bottom of the esophagus or in a hiatal hernia.
To further illustrate this point, let’s look to research on this.
Smith and colleagues (1998) studied people with lower esophageal mucosal rings. Out of 26 people with rings, 16 caused food impaction, but only 12 had the sensation of this dysphagia to solids. Nine out of the 12 (75%) pointed to the suprasternal notch/sternal angle or above (with 7 pointing higher up in the neck). None of these 12 actually had any pharyngeal or cervical esophageal abnormalities, showing it is a referred sensation from the problem at the bottom of the esophagus. Only 3 of the 12 (25%) symptomatic people correctly localized the food to mid to low chest.
Similarly and more recently, Marvin & Thibeault from the University of Wisconsin-Madison presented at the Dysphagia Research Society’s meeting (Baltimore, 2018) on people’s accuracy of localizing pharyngeal versus esophageal residue or hold-up (also called “stasis”). They performed a prospective analysis of all patients (387) who complained of bolus stasis (food/liquid stuck) on their intake questionnaires. Based on their standard of care, they performed a combined videofluoroscopic swallow study (VFSS) and an esophagram. Only 34% accurately identified the location of where the bolus was stuck. Accuracy was better when the person thought that the problem was in the esophagus, as 79% of the abnormalities were indeed in the esophagus, and none of these people who pointed to the esophagus had any pharyngeal problems. However, 41% of those who localized the problem to the neck or pharynx actually had problems in the esophagus. This is that referred sensation again.
Many of these people with esophageal dysphagia will end up at a typical videofluoroscopic swallow study (VFSS), and the SLP may tell them they have a normal swallow due to not fully evaluating the whole swallowing chain from the mouth to stomach. Ekberg’s editorial suggested that we should only focus our diagnostics on the patient’s symptoms. Do you want to miss dysphagia in 41% of people referred to you?
In Multiphase Dysphagia Evaluations, Esophageal Sweeps Are Not Screens
Let’s get the semantics straight right away: This esophageal sweep is NOT a “screen.” As noted by radiologist, Cheri L. Canon, MD, FACR (professor and Witten-Stanley Endowed Chair of Radiology at the University of Alabama at Birmingham), we should NOT call the esophageal component of our VFSS a screen. She spoke on this topic at the 2016 Dysphagia Research Society’s Post-Graduate Course.Giselle Carnaby, MPH, PhD, FASHA agreed with Canon at the same 2016 Dysphagia Research Society’s Post-Graduate Course. Both Canon and Carnaby noted that by definition: a screen is used to recognize a problem in a non-referred population. For example, all women get screened for breast cancer with a mammogram. When we are performing a VFSS, we already have a person referred to our swallowing service due to an observed, suspected or perceived difficulty swallowing. Therefore, we owe it to our patients to not just screen the swallow. We are specifically challenging the patient and thoroughly performing a multiphase dysphagia evaluation, looking all phases for what is normal and abnormal. That is NOT a screen. (See my Medbridge Education article called Good Dysphagia Evaluation Guides Treatment (Part 2)).
So, we call the esophageal examination a scan or a sweep, and it is crucial. Canon, the radiologist mentioned above, agreed with the use of the esophageal scans during our VFSS as they add so much to our therapeutic recommendations regarding esophageal clearance, knowing that we will refer for further testing if suspicions are high for esophageal dysphagia. JoAnne Robbins, PhD, CCC-SLP, BCS-S, also at the 2016 Dysphagia Research Society Annual Meeting, stated that esophageal testing is:
“terribly important in older people to rule-out pneumonia contributed to by what is going on lower down.”
Okay, now that I have regurgitated that, I can move on…
Good Accuracy with MBSS/VFSS Plus Robust Esophageal Sweeps
In 2012, Gullung & colleagues (including Dr Bonnie Martin-Harris, founder of the Modified Barium Swallow Impairment Profile/MBSImP) found that the esophageal clearance scores on the MBSImP were closely associated with abnormal esophageal findings on High Resolution Manometry (HRM with Impedance Testing). Per this study, 78% of people with a confirmed esophageal abnormality on HRM also had an abnormal esophageal retention rating on the MBSImP esophageal scanning with boluses of nectar thick/mildly thick liquid and barium pudding. Authors stressed that findings of esophageal retention on the MBSImP warrant further esophageal testing. They highlighted the importance of a thorough examination.
Richter shared research happening at USF during his Dodds Donner lecture. The USF team also presented a poster at DRS in 2019. I was excited to hear about this research and read their 2019 publication reinforcing the need for SLPs to perform more thorough esophageal scanning with foods, liquids and pills (see Watts, et al., 2019). Their study analyzed 307 modified barium swallow studies. It was a retrospective analysis of consecutive outpatients with a mean age of 61. SLPs and radiologists had good inter-rater reliability once clear operational definitions were established.
Watts and colleagues found that 80 out of 307 people had esophageal dysphagia per their esophageal sweeps. That is 26% of their outpatient population. Do you want to miss 1 in every 4 causes of dysphagia by not thoroughly scanning the esophagus? Scanning these 80 people allowed for prompt and appropriate referrals, and 42 of them had subsequent examinations (i.e., timed barium esophagram, double contrast barium esophagram, high resolution manometry, endoscopy). In the 42 people who had further testing, 100% of them had positive esophageal findings. A prompt referral leads to quick management. Forty-three people had multi-phase dysphagia, meaning abnormalities in the oropharynx and esophagus. Out of the people who had no oropharyngeal impairment, 37 actually had problems in the esophagus. That means that if you do not scan down the esophagus during your routine protocol for your VFSS, you would have missed those 37 people whose safety, quality of life and nutritional intake were being impacted by dysphagia on potentially a daily basis.
Per the poster presented at DRS in 2019 in San Diego by Watts and colleagues, the diagnostic accuracy of the esophageal sweeps was high when compared with same day formal esophageal testing (timed barium emptying studies, high resolution manometry, and/or EGD/ esophagogastroduodenoscopy). In the 73 people tested with the esophageal sweep protocol, the sensitivity for detecting an esophageal abnormality was 89%. The specificity was 83%. In other words, when the esophageal sweep was positive in 44 people, the formal esophageal testing confirmed that 39 people did indeed have an esophageal abnormality. The team noted that the sweep missed some incidences of ineffective esophageal motility (IEM), “jackhammer esophagus,” and esophageal junction outflow obstruction.
Esophageal Dysphagia is Quite Common
I recalled another study on this topic presented at the 2016 Dysphagia Research Society meeting. This study was by SLPs and the medical doctor from MassTex Imaging, LLC, a mobile videofluoroscopic swallow study company in New England. Litwack and colleagues (2016, March) analyzed 10,569 electronic medical records, finding 9,921 consecutive patients who had both an MBSS and an esophagram (MD on board the mobile units). They noted that the only time they do not scan down is when there are significant seating or positioning limitations which preclude both the anterior-lateral and lateral views of the esophagus. Unlike the Watts’ study, these patients were mainly from nursing facilities and rehabilitation centers with a mean age of 81. The researchers were surprised at how common esophageal abnormalities were (per personal communication with Amy Litwack on May 31, 2019). Esophageal dysphagia was a more common finding than aspiration (47% for esophageal versus 35% for aspiration). The most common esophageal problems were due to impaired esophageal motility (36%) with findings of slow bolus transit and bolus retention/stasis. Structural/anatomic abnormalities were seen in 10% of the patients, such as a cricopharyngeal bar, Zenker’s Diverticulum, other diverticuli, hiatal hernia, and obstruction. They were able to provide diet and specific swallowing strategy recommendations in 20% of the patients (e.g., alternating solids and liquids during meals, sitting upright during the meal, and remaining upright 30 minutes after a meal – to name a few). Litwack noted that out all of those patients, that is a lot of important esophagus-directed recommendations provided by the SLP. In addition to specific recommendations, the SLPs take action with appropriate referrals. For example, when severe gastro-esophageal outlet obstruction was found in a very small percentage, they were rapidly referred for further diagnosis and intervention.
Miles and colleagues (2015) added esophageal visualization with a large liquid barium bolus and a barium capsule to their videofluoroscopic swallow studies. They studied a convenience sample of consecutive patients referred to their clinic by otolaryngology or by a speech-language pathologist. Out of 111 people, 68% had abnormal esophageal findings. Interestingly, 1/3rdof those people only had this esophageal abnormality. I have found this to be typical in outpatients coming for videofluoroscopic swallow studies. Just imagine the dysphagia that goes unidentified if a swallow study stops at the top of the esophagus.
Modernize the Videofluoroscopic SwallowStudy with Multiphase Dysphagia Evaluations
Watts and colleagues advise that the MBSS/VFSS has to be “modernized.” A “robust esophageal sweep protocol” (also called REST – Robust Esophageal Sweep Test– by Dr Richter during his Dodds Donner lecture) can “reduce the risk that the etiology of the swallowing complaint goes undetected and thus untreated.” (Quotes from Watts, et al. 2019, p 40.)
To reiterate, this modernized MBSS/VFSS with thorough esophageal sweeps does not replace more thorough analysis of the esophagus, rather it immediately highlights the need for appropriate referrals for further testing (e.g., with endoscopy, high resolution manometry, and barium swallow/esophagrams).
Ekberg (2019) pointed out that the Watts’ study “has no clue about false negatives,” meaning they do not know if their robust esophageal sweep may have missed some people, labeling a person with a “normal” esophagus when there really is a problem. The Watts, et al., 2019 poster showed that the esophageal sweep was only negative 5 times out of 44, when the formal esophageal testing showed the condition to be present. Richter also seemed to indirectly respond to that issue during his lecture when he stated:
“If you don’t look, you have a 0% chance of finding it.”
So that is even more false negatives if you are doing a VFSS without scanning down the esophagus throughout your study. Another way of thinking about it, per Richter, is: “If you don’t look, you miss it 100% of the time.” Additionally, when the SLP sweeps the esophagus, if there is any indication that the bolus is not clearing, the SLP would make a referral.
The Pharynx and the Esophagus are Inter-Related
This is not a new revelation, but it gets even more intriguing. Keep reading.
Richter recommended a 1985 paper by Dr Bronwyn Jones, MD, FRACP, FRCR and colleagues from Johns Hopkins (including Dr Martin Donner) titled: “Pharyngoesophageal Inter-relationships.” The authors noted:
“changes in pharyngeal structure and function can result from esophageal disease.”
So, this is the esophagus affecting the pharynx, but I would also say: “and vice-versa.” Let’s look at both.
Pharynx Affects the Esophagus
Consider how poor pharyngeal functioning can cause poor esophageal motility and emptying. A poor pharyngeal stripping wave (poor pharyngeal constriction) and lingual propulsion can set up a sluggish peristaltic wave that carries throughout the esophagus. Please also see my prior esophageal blog, where Ashli O’Rourke, MD (otolaryngologist) noted that the double swallow, if done within 10 seconds of the primary swallow, can halt the secondary peristaltic clearing wave in the esophagus.
The Watts, et al. (2019) article makes this point when referring to a study that found 87% of head and neck cancer survivors have co-occurring esophageal dysphagia (Farwell, D.G et al. 2010). Farwell and colleagues (2010) from UC Davis Department of Otolaryngology found that only 13% of their patients who had head and neck cancer had a normal esophagoscopy. They scoped the esophagus in 100 people who were 40 months post a variety of treatments for mostly advanced stage cancer of oral cavity, oropharynx, nasopharynx, hypopharynx and larynx. Structural esophageal findings were: peptic esophagitis, stricture, candidiasis, Barrett’s metaplasia, gastritis and carcinoma (in that order of frequency of occurrence). Who knows what other motility issues may have been co-occurring, as the testing was just via endoscopy and not via a barium swallow or high resolution manometry (HRM)?
Back in 1985, the Jones, et al. article instructed on the “performance inter-relationships between the pharynx and esophagus” and stated:
Swallowing evaluations “should always examine the entire swallowing tract, including the mouth (p 225).”
“Examination of the whole swallowing chain is necessary instead of focusing on the symptomatic region (p 232).”
I love that concept of the “whole swallowing chain!” It reinforces how linked it all is.
Esophagus Affects the Pharynx
Dr Bronwyn Jones and colleagues (1985) further illustrated this point with discussing their study of 124 individuals (excluding 35 with known neuromuscular diseases and laryngectomy) to stress the importance of understanding the effect of esophageal disease on the cricopharyngeal muscle and the pharynx. A prominent cricopharyngeus may point to an esophageal abnormality or significant reflux disease. They noted that the higher up the esophageal distention is by liquid stasis (retention), the greater the pressure is at the cricopharyngeal muscle, potentially in order to protect the airway just above the top of the esophagus. This may lead to a prominent or tight cricopharyngeal muscle over time (aka, hypertrophy of the cricopharyngeus muscle). They found an esophageal abnormality in 23 of the 24 consecutive patients with cricopharyngeal prominence (e.g., spasm, acid sensitivity, hiatal hernia, reflux and retrograde flow in many cases up to the pharyngoesophageal segment, Schatzki’s ring, severe esophagitis, webs, and absent peristalsis). In this same group of 24 people, 11 had other pharyngeal dysphagia, including 7 with lateral pharyngeal pouches. In another study at their swallowing center which studied 11 people with Zenker’s and 16 people with lateral pharyngeal pouches, the findings of esophageal dysphagia was significant. Only 1 of the 16 people with pharyngeal pouches (pharyngoceles) had a normal esophagus. Most of the people had esophageal dysmotility and reflux. All 11 people with Zenker’s diverticulum had esophageal abnormalities, and not just prominent cricopharyngeal muscles.
These numbers from the 1985 studies at Johns Hopkins were an eye-opener to me in 2019. We often receive referrals from our otolaryngology team regarding cricopharyngeal dysfunction and suspected pharyngoceles from their direct endoscopic evaluations.
Therefore, my take-home message is:
Do not only look at the referred zone or the area of complaint. Maybe we overly focus on the pharynx when a patient is referred by otolaryngology with history of head and neck cancer patient, pharyngoceles, or a cricopharyngeal dysfunction. Instead, make sure to evaluate the whole swallowing chain, especially the esophagus.
Summary on Comprehensive Multiphase Dysphagia Evaluations
“SLPs are positioned to manage multiphase assessments,” Richter concluded in his 2019 DRS Dodds Donner Lecture.
Similarly, he and his colleagues concluded in the Watts 2019 article (p 40):
“Given objective guidelines and additional training, the SLP has the unique opportunity to improve the diagnostic accuracy of the MBS (VFSS) by adding a standardized esophageal sweep protocol to the routine MBS (VFSS) assessment.”
“Since swallowing is a multi-phase phenomenon, swallow evaluation should be comprehensive across all phases.” (Watts, et al., 2019, p 35)
How I Can Learn More
Richter notes that our ASHA Scope of Practice includes esophageal dysphagia, and the ASHA Practice Portal may be a great resource for support in learning more about the esophagus. See also terminology clarifications in the addendum section below.
The multidisciplinary Dysphagia Research Society has been a great resource for me. It is a think-tank of researchers, clinicians and students who work with people across the life-span. It is made up of radiologists, otolaryngologists, gastroenterologists, pediatricians, speech-language pathologists, and more – allowing all of the disciplines passionate about dysphagia to collaborate and learn from each other.
Your facilities should include esophageal components in your competency checklists for the VFSS. Richter advises clinicians to stay up-to-date with emerging research. Barriers are inconsistent training in universities and on-the-job. Insurance can be a barrier, as some do not allow for VFSS and Barium Swallow testing on the same day, making comprehensive testing challenging for people. There is also not full consensus within radiology to include thorough esophageal sweeps in the VFSS. Certainly, there needs to be ongoing multidisciplinary collaboration to make sure our multiphase dysphagia evaluations are comprehensive to include esophageal sweeps. Hopefully, this article will continue the conversation started by prominent radiologists, gastroenterologists, otolaryngologists and speech-language pathologists in our field. Thank you in advance for commenting below.
Here is that link again to my prior blog on esophageal dysphagia from 2014.
See also this blog on Reflux (GERD and LPR).
References:
Ekberg, O. (2019). To sweep or not to sweep. Dysphagia, 34, 1. https://link.springer.com/article/10.1007/s00455-018-09967-4
Farwell, D.G., Rees, C.J., Mouadeb, D.A., Allen, J., Chen, A.M., Enepekides, D.J. & Belafsky, P.C. (2010). Esophageal pathology in patients after treatment for head and neck cancer. Otolaryngology Head and Neck Surgery, 143(3), 375-8. https://www.ncbi.nlm.nih.gov/pubmed/20723774
Gullung, J.L., Hill, E.G., Castell, D.O. & Martin-Harris, B. (2012). Oropharyngeal and esophageal swallowing impairments: There association and the predictive value of the modified barium swallow impairment profile and combined multichannel intraluminal impedance-esophageal manometry. Ann Otol Rhinol Laryngol., 121(11), 738-45.
Humbert, I.A., Michou, E., MacRae, P.R. Crujido, L. (2012). Electrical stimulation and swallowing: How much do we know? Seminars in Speech & Language, 33(3), 203-216.
Jones, B., Ravich, W.J., Donner, M.W., Kramer, S.S. & Hendrix, T.R. (1985). Pharyngoesophageal interrelationships: Observations and working concepts. Gastrointestinal Radiology, 10, 225-233. https://www.ncbi.nlm.nih.gov/pubmed/4029538
Levine, M.S., Rubesin, S.E. & Laufer, I. (2009). Barium studies in modern radiology: Do they have a role? Radiology, 250,18-22.
Litwack, A., Arsenault, J.K., Brand, S., Morgan, L. & Baumer, J. (2016, March). Prevalence of esophageal findings in adults via MBS with esophageal assessment. Poster presented at the Dysphagia Research Society Annual Meeting, Tucson, AZ.
Marvin, S. & Thibeault, S. (2018, March). Pharyngeal versus esophageal stasis: Accuracy of location. Session presented at Dysphagia Research Society Annual Meeting, Baltimore, MD.
Miles, A., McMillan, J., Ward, K. & Allen, J. (2015). Esophageal visualization as an adjunct to the videofluoroscopic study of swallowing. Otolaryngol Head Neck Surg, 152(3), 488-93. https://www.ncbi.nlm.nih.gov/pubmed/25605697
Miles, A. (2017). Inter-rater reliability for speech-language therapists’ judgment of oesophageal abnormality during oesophageal visualization. Int J Lang Commun Disord, 52(4), 1-6. https://www.ncbi.nlm.nih.gov/pubmed/27624620
Smith, D.F., Ott, D.J. Gelfand, D.W. & Chen, M.Y. (1998). Lower esophageal mucosal ring: Correlation of referred symptoms with radiographic findings using a marshmallow bolus. AJR Am J Roetgenol. 171(5), 1361-5.
Watts, S., Gaziano, J., Jacobs, J. & Richter, J. (2019). Improving the diagnostic capability of the modified barium swallow study through standardization of an esophageal sweep protocol. Dysphagia, 34, 34-42. https://www.ncbi.nlm.nih.gov/pubmed/30635777
Watts, S., Gaziano, J., Kumar, A. & Richter, J. (2019, March). The diagnostic accuracy of an esophageal sweep protocol. Poster presented at Dysphagia Research Society Annual Meeting, San Diego, CA.
Read more about the history of the Barium Swallow and what it can detect:
- Levine, M.S. & Rubesin, S.E.. (2017). History and Evolution of the Barium Swallow for Evaluation of the Pharynx and Esophagus. Dysphagia, 32(1), 55-72. https://doi.org/10.1007/s00455-016-9774-y
Addendum: Notes on Terms/Examinations
The terms modified barium swallow study (MBSS) and the videofluoroscopic swallow study (VFSS) are the same, and the terms are used interchangeably. You may also hear videoswallow study. This is the study directed by the speech-language pathologist with a radiologist or radiology technician in the room operating the camera. If the radiologist is not in the room, they will dictate their report upon review of the images and the SLP’s written or verbally communicated findings. When the radiologist is not in the room, the SLP needs to communicate any concerning findings with the radiologist, as the SLP cannot diagnose the underlying medical problem. The radiologist’s report should always refer the reader to the SLP’s note for more details, as it is the SLP who analyzes all the components of the swallow. The MBSImP has 17 components that we rate based on our real-time, slow-motion and frame-by-frame analysis of the images after the study.
The barium swallow/esophagram does not evaluate the oral preparatory, oral or pharyngeal phases, and it does not always detect penetration and aspiration. It cannot indicate why someone is having residue or aspiration, especially when only still images are saved in a series, and a fluoro loop/video is not recorded at 30 frames per second. It is primarily focused on the esophagus through the stomach (to the small bowel if a small bowel follow-through is also ordered). It analyzes the fully distended esophagus, esophageal structure and motility, esophageal emptying and reflux. Can the patient take enough barium with consecutive sip/swallows to fully distend the esophagus? Can they stand, or do they have to lay down on a potentially hard table? The barium swallow may be a timed barium esophagram, and it uses single or double-contrast liquid barium. Sometimes the barium swallow will administer a pill to catch smaller strictures or rings, but this is not always standard; therefore, I think it should be specifically requested.
The barium swallow does not test foods, which makes the test not as useful if someone’s specific complaints are with foods getting stuck. Therefore, the modernized MBSS/VFSS proposed by Richter with the robust esophageal sweep with foods, liquids and pill is the most comprehensive mouth to distal esophageal evaluation. Dr JoAnn Robins (my professor of dysphagia from the University of Wisconsin-Madison back in the 1990’s) called this an “oro-esophagram” for years. This indicates that some SLPs have been focused on the mouth to the stomach for years. Since 1999 when I started doing videofluoroscopic swallow studies, I have been scanning the esophageal. It is within the SLP’s scope of practice to evaluate the esophagus and provide safe swallowing strategies to promote functional esophagus clearance. It is important for the SLP to at least comment on:
- slow emptying,
- bolus stasis/bolus retention (how might dry mouth/mucosa and poor dentition impact),
- what works to clear the bolus, and
- presence of any retrograde flow and up to what level (below the pharyngoesophageal segment/UES or through the UES).
Did the liquid come back up to the top of the esophagus or backflow out of the esophagus into the pharynx and over into the larynx/airway?
Is there a significant risk for aspiration after the swallow?


Extremely informative.